The clinical role of PET/MRI is evolving rapidly in breast cancer, according to two studies presented at the European Society of Breast Imaging (EUSOBI) annual meeting, which took place recently in Aberdeen, U.K.
In patient treatment, there is a shift to neoadjuvant chemo(targeted) therapy (NAC), with less invasive surgery and response monitoring using MRI. A pathologic complete response (pCR) after NAC can lead to an improved prognosis, as does metabolic/radiologic complete response (mCR/rCR) after NAC, Melissa Lenaerts, PhD, from the Department of Surgery, Maastricht University Medical Center, the Netherlands, and colleagues pointed out.
The aim of their study was to investigate the prognostic value of molecular and radiologic characteristics of the primary tumor and axillary lymph nodes (ALNs) on dedicated breast F-18 FDG PET/MRI for event-free survival (EFS; recurrence and/or death) in breast cancer patients treated with NAC.
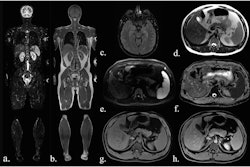
 Dedicated breast F-18 FDG PET/MRI exam pre- (A, D, G), mid- (B, E, H), and post-NAC (C, F, I) of a 41-year-old patient diagnosed with a triple negative (TN), grade 2, invasive carcinoma. The SUVmax values of the primary tumor were 14.68 pre-NAC, 1.69 mid-NAC, and 1.87 post-NAC, while SER values were 1.19, 0.52, and 0.63, respectively. Figure courtesy of Melissa Lenaerts, PhD, Dr. Thiemo van Nijnatten, PhD, et al and presented at EUSOBI 2025.
Dedicated breast F-18 FDG PET/MRI exam pre- (A, D, G), mid- (B, E, H), and post-NAC (C, F, I) of a 41-year-old patient diagnosed with a triple negative (TN), grade 2, invasive carcinoma. The SUVmax values of the primary tumor were 14.68 pre-NAC, 1.69 mid-NAC, and 1.87 post-NAC, while SER values were 1.19, 0.52, and 0.63, respectively. Figure courtesy of Melissa Lenaerts, PhD, Dr. Thiemo van Nijnatten, PhD, et al and presented at EUSOBI 2025.
Between 2015 and 2017, patients diagnosed with cT2-4N0 or cT1-4N1-3 underwent dedicated breast F-18 FDG PET/MR imaging pre-, mid-, and post-NAC for response assessment. For each patient, follow-up data on recurrence and death were collected up to April 2024. Using univariable Cox regression and Kaplan-Meier analysis, the researchers evaluated the association between molecular (PET-derived) and radiologic (MRI-derived) characteristics of the primary tumor and ALNs and the probability of EFS.
A total of 41 patients with 42 breast tumors underwent dedicated breast F-18 FDG PET/MRI pre-, mid-, and post-NAC for response assessment. The median follow-up time was nine years.
Univariable Cox regression showed no significant association between pre- and mid-NAC PET- and MRI-derived parameters and EFS, the researchers said. Post-NAC, they found a significantly (p < 0.1) positive association with recurrence and/or death for the maximum standardized uptake value (SUVmax; hazard ratio [HR] 1.41 [90% confidence interval [CI] 1.089-1.831], p = 0.029), SUVpeak (HR 1.79 [90% CI 1.138-2.828], p = 0.035), SUVmean (HR 1.8 [90% CI 1.110–2.930], p = 0.046), tumour size (HR 1.04 [90% CI 1.002-1.082], p = 0.087), and signal enhancement ratio (SER; HR 6.46 [90% CI 1.111-37.511], p = 0.081) of the primary tumor.
“For mid-NAC and post-NAC, patients with SUVmax above the median value tend to have higher risk of recurrence and/or death compared to patients with lower SUV value,” they noted. “Regarding post-NAC SER, patients with a value above the median also tend to have a poorer EFS compared to patients with lower SER values. However, none of the observed differences were statistically significant.”
Preoperative axillary staging
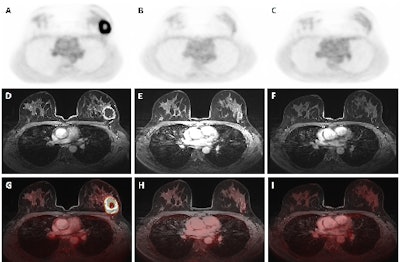
F-18 FDG PET/MRI is also helping to optimize axillary lymph node management, Dr. Daniela Ballerini, a radiologist in the Breast Radiology Unit at the IRCCS Ospedale San Raffaele in Milan, and colleagues stated in another EUSOBI 2025 presentation.
Previous research shows that omitting axillary surgery is a safe option for patients with small breast cancers and negative preoperative axillary ultrasound scans, but clinical implementation has been hindered by concerns over the loss of pathological data on positive nodes and their therapeutic implications. To facilitate the shift from surgery to imaging, effective diagnostic tools are needed to provide reliable information on nodal status while omitting axillary surgery, they explained.
The Milan team evaluated the accuracy of hybrid F-18 FDG PET/MRI in detecting axillary lymph nodes macro-metastases, in order to safely evaluate in the future axillary surgery omission in selected early breast cancer patients, in a prospective interventional single-arm monocentric trial.
Between June 2020 and April 2024, the group recruited 246 patients with breast cancer (251 axillae evaluated due to five having bilateral disease) without nodal involvement on ultrasound and clinical examination. They were eligible for upfront surgery. All the patients underwent F-18 FDG PET/MRI before surgery. Two radiologists and two nuclear medicine physicians, all blinded, independently reviewed the images.
The mean (SD) age at surgery was 56.3 (10.7), and the mean (SD) tumor size was 17.5 (13) mm at final pathology, the authors wrote. Macrometastatic axillary lymph nodes were found at surgery in 61 cases (24.3%). F-18 FDG PET/MRI had identified 43 (70.5%) of these cases. The hybrid technique significantly outperformed both F-18 FDG PET and MRI alone, which identified 36 (59%; p = 0.016) and 25 (41%; p < 0.001) cases, respectively. Negative predictive value was higher for F-18 FDG PET/MRI (89.4%) than F-18 FDG PET (86.4%, p = 0.021) and MRI (82.9%, p < 0.001) alone.
Prior to surgery, F-18 FDG PET/MRI detected 70.5% of cases with macrometastatic axillary lymph nodes in patients with clinically negative axilla, with greater accuracy than F-18 FDG PET or MRI alone.
“In the future, the surgical staging of axillary nodes of early breast cancer patients might be replaced by AI-assisted diagnostic tools capable of accurately predicting axillary status by integrating clinicopathological data with imaging and molecular signatures,” they concluded. “This integrated approach could combine both predictive and prognostic data, thus further refining personalized treatment strategies.”
You can read the full Dutch EUSOBI poster here. The co-authors were Drs. Cornelis de Mooij, Janneke B. Houwers, Cristina Mitea, Marco Panosetti, Maaike de Boer, Kristien B.M.I. Keymeulen, Felix Mottaghy, Marc B.I. Lobbes, Patty Nelemans, Marjolein Smidt, Thiemo van Nijnatten.
You can view the Italian EUSOBI poster here. The co-authors were Drs. Rosa Di Micco, Carolina Santangelo, Claudio Losio, Maria Grazia Rodighiero, Simona Tacchini, Sabrina Calamará, Elena Venturini, Michele Colombo, Giulia Cristel, Veronica Zuber, Oreste Gentilini, and Pietro Panizza.