MRI is proving crucial for detecting both parenchymal and nonparenchymal brain metastases, including those at extracranial sites, award-winning Spanish experts have reported.
“Systematic MRI assessment, guided by a structured checklist and specialized imaging techniques, improves detection accuracy,” noted Dr. Zhao Hui Chen Zhou, from the Neuroradiology Section in the Department of Radiology at Madrid’s Hospital Universitario 12 de Octubre, and colleagues. “This approach minimizes missed diagnoses and supports precise, timely interventions, ultimately improving outcomes for patients with metastatic disease.”
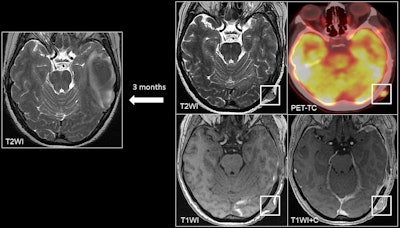 A 45-year-old patient with melanoma presented with a left temporal hemorrhagic metastasis. At the 3-month follow-up, a left occipital cutaneous/subcutaneous metastasis appeared as a soft tissue lesion with contrast enhancement on postcontrast T1 sequences and on PET/CT.All figures courtesy of Dr. Zhao Hui Chen Zhou et al and presented at ECR 2025.
A 45-year-old patient with melanoma presented with a left temporal hemorrhagic metastasis. At the 3-month follow-up, a left occipital cutaneous/subcutaneous metastasis appeared as a soft tissue lesion with contrast enhancement on postcontrast T1 sequences and on PET/CT.All figures courtesy of Dr. Zhao Hui Chen Zhou et al and presented at ECR 2025.
MRI is the standard imaging method for detecting brain metastases and is used increasingly due to the availability of guidelines and recommendations for screening and follow-up, according to the authors, who received a cum laude award from the ECR 2025 e-poster judges.
“Metastases visible on cranial MRI are not confined to the brain's parenchyma; up to 20% of them can be found in nonparenchymal areas, which may include both intracranial and extracranial structures. Therefore, it is essential to have a checklist to ensure that all structures are thoroughly examined and nothing is overlooked,” they explained.
Bone metastases are the most common nonparenchymal metastases, and the three most common primary cancers occur in the breast, lung, and prostate. Depending on the anatomy, skull-base metastases may present as five clinical syndromes. The most common mechanism is hematogenous spread, and another possible mechanism is retrograde venous spread via the valveless Batson's venous plexus, the researchers stated.
Bone metastases may present as diffuse bone involvement or focal lesions, where the hyperintense signal from fatty marrow on T1-weighted imaging (T1WI) sequences without fat suppression is replaced by a hypointense lesion. Lytic bone metastases show restriction in diffusion-weighted imaging (DWI) -- especially of breast and lung cancer origin -- but DWI is not useful for prostate bone metastases. Bone metastases show variable contrast enhancement, and postcontrast sequences allow the assessment of whether there is associated dural invasion.
“Use fat saturation pulses when obtaining postcontrast T1WI,” they recommended, adding that subtraction sequences may also be helpful.
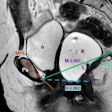
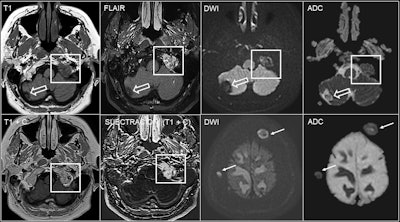 60-year-old woman with breast cancer and bone metastases in the left occipital condyle (square) showing a hypointense focal lesion on T1 sequences without contrast, hyperintense signal on FLAIR sequences and diffusion restriction. Contrast enhancement can be seen on postcontrast 3D T1-weighted sequences, where subtraction sequences may be helpful if fat suppression has not been performed. There is also a cavernoma (empty arrow) in the right cerebellar hemisphere and other bone metastases with diffusion restriction in the calvarium (arrows).
60-year-old woman with breast cancer and bone metastases in the left occipital condyle (square) showing a hypointense focal lesion on T1 sequences without contrast, hyperintense signal on FLAIR sequences and diffusion restriction. Contrast enhancement can be seen on postcontrast 3D T1-weighted sequences, where subtraction sequences may be helpful if fat suppression has not been performed. There is also a cavernoma (empty arrow) in the right cerebellar hemisphere and other bone metastases with diffusion restriction in the calvarium (arrows).
Leptomeningeal carcinomatosis (LMC) is a rare but serious complication that occurs in about 5% to 8% of patients with solid tumors, and it is caused by the spread of tumor cells into the leptomeninges and subarachnoid space. The most common primary is breast cancer, followed by lung cancer and melanoma, they continued.
Multifocal clinical deterioration is highly suggestive of LMC, but patients may present with isolated or subtle neurological symptoms or signs and even have a normal neurological examination. “It is recommended to perform an MRI before conducting a lumbar puncture, if possible, as the procedure can lead to dural enhancement,” the authors noted.
Dural metastases are very rare, accounting for 1% of intracranial tumors, and they can occur through direct spread from a bone metastasis, via hematogenous spread, or in a small percentage of cases by intraoperative dissemination. The most common primaries are breast, prostate, and lung.
Diffuse dural thickening and enhancement may occur, and it can appear smooth or nodular. Focal dural mass mimicking meningioma may be seen, and in these cases, it is not easy to differentiate between the two entities on conventional MRI, they added.
On PET imaging with gallium-68 DOTATATE, meningiomas usually show high uptake because they contain somatostatin receptors. “However, caution is advised, as metastases from neuroendocrine tumors also show high uptake. Meningiomas are typically characterized by a complete ring or > 50% enhancement on the postcontrast FLAIR sequence (‘CE-FLAIR rim sign’),” the Madrid researchers pointed out.
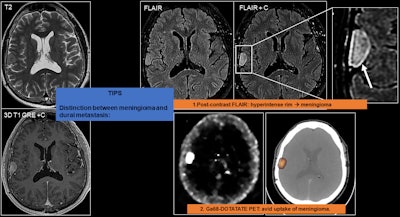 The main differential diagnosis of focal dural metastasis is a meningioma, which is much more common, and they are difficult to differentiate on conventional MRI. To help differentiate them, postcontrast fluid attenuated inversion recovery (FLAIR) sequences can be used. Meningiomas may show up as a hyperintense rim on FLAIR MRI and Ga-68 DOTATATE PET, as meningiomas show intense uptake due to the presence of somastotatin receptors.
The main differential diagnosis of focal dural metastasis is a meningioma, which is much more common, and they are difficult to differentiate on conventional MRI. To help differentiate them, postcontrast fluid attenuated inversion recovery (FLAIR) sequences can be used. Meningiomas may show up as a hyperintense rim on FLAIR MRI and Ga-68 DOTATATE PET, as meningiomas show intense uptake due to the presence of somastotatin receptors.
Pituitary metastases are rare, comprising 0.4% of intracranial metastases and about 1% to 3.6% of operated pituitary lesions. The most common primaries occur in the breast, lung, kidney, and prostate, and most are asymptomatic and are discovered incidentally on imaging. The most common clinical presentation is diabetes insipidus and panhypopituitarism, reflecting a predilection for involvement of the neurohypophysis and pituitary stalk, they wrote.
Pineal gland metastases occur in 0.4% to 3.8% of cancer patients, with the most common primaries occurring in the lung and breast. Most pineal metastases are asymptomatic, although they may clinically present with headache, encephalopathy, and hydrocephalus. Identifying pineal metastases is crucial, as they can lead to leptomeningeal dissemination, which occurs in up to 67% of cases, they added.
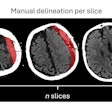
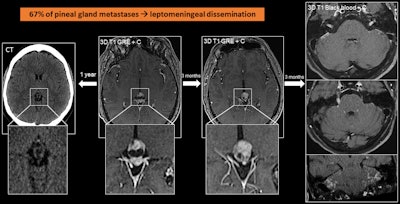 A 56-year-old man with lung cancer with pineal metastasis, which appears as a complex cystic lesion with a solid anterior pole. This finding, which was not present in a CT scan obtained a year earlier, progressed in the MRI scan after three months. In the following months, he developed leptomeningeal dissemination.
A 56-year-old man with lung cancer with pineal metastasis, which appears as a complex cystic lesion with a solid anterior pole. This finding, which was not present in a CT scan obtained a year earlier, progressed in the MRI scan after three months. In the following months, he developed leptomeningeal dissemination.
“Like pituitary metastases, they are not easy to differentiate from other lesions,” the researchers stated. “Suspect when there are new pineal lesions in patients with lung and breast cancer.”
Cutaneous and subcutaneous soft tissue metastases are rare, accounting for approximately 0.7% to 10% of cases, but usually indicate widespread metastatic disease and a poor prognosis. Primary sites vary according to gender, with the most common sites in women being breast, lung, gynecological, and gastrointestinal (in decreasing order), and in men being lung and gastrointestinal, they wrote.
These metastases may present as generally small nodules (< 2 cm) or infiltrative masses with homogeneous or heterogeneous enhancement. Imaging is not specific but must be considered in the context of a history of systemic cancer, and biopsy is mandatory in cases where there is no known primary tumor.
You can read the full prize-winning exhibit on the EPOS database of the ESR. The work was presented at ECR 2025. The co-authors were A. Hilario Barrio, E. Salvador, A. Cardenas, J. Romero Coronado, C. Lechuga Vázquez, A. Martínez de Aragón Calvo, A. Ramos Gonzalez