MRI-identified bladder wall invasion was found to be a consistent predictor of tumor recurrence and tumor-related mortality from uterine cervical cancer and may replace cystoscopy in the preoperative staging, according to a study published in European Radiology on 4 October.
The authors, led by Dr. Matteo Bonatti of the radiology department of Paracelsus Medical University in Bolzano, Italy, noted that the MRI-based approach could reduce costs and expedite staging in replacing cystoscopy.
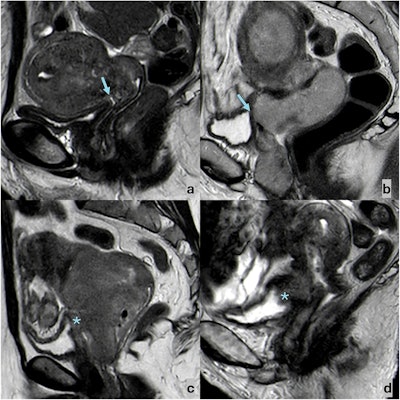 Sagittal T2-weighted FSE images showing the possible appearances of bladder wall–cervical cancer relation. (a) A fatty cleavage plane (arrow) may be observed between CC and the bladder, which shows a thin T2-hypointense wall. (b) The fatty cleavage plane between CC and the bladder is obliterated (arrow), but the bladder wall appears thin and T2-hypointense. (c) The fatty cleavage plane between CC and the bladder is obliterated, and the bladder wall appears thickened, with intermediate signal intensity (star). (d) The fatty cleavage plane between CC and the bladder is obliterated, the bladder wall appears thickened, with intermediate signal intensity, and neoplastic tissue protrudes in the bladder lumen (*).Bonatti et al; European Radiology
Sagittal T2-weighted FSE images showing the possible appearances of bladder wall–cervical cancer relation. (a) A fatty cleavage plane (arrow) may be observed between CC and the bladder, which shows a thin T2-hypointense wall. (b) The fatty cleavage plane between CC and the bladder is obliterated (arrow), but the bladder wall appears thin and T2-hypointense. (c) The fatty cleavage plane between CC and the bladder is obliterated, and the bladder wall appears thickened, with intermediate signal intensity (star). (d) The fatty cleavage plane between CC and the bladder is obliterated, the bladder wall appears thickened, with intermediate signal intensity, and neoplastic tissue protrudes in the bladder lumen (*).Bonatti et al; European Radiology
The findings of the study show that while bladder wall invasion seen on MRI is an independent risk factor for both recurrence and mortality, cystoscopy-defined bladder mucosa infiltration was not an independent risk factor for either recurrence or mortality.
The Italian multicenter retrospective study included 214 women who had undergone MRI staging for histologically confirmed cervical cancer. Patients were from two centers: 103 from Center A; 111 from Center B. The patients ranged in age from 47 to 65, with a median age of 55. Histology showed that 185 (86.4%) of the neoplasms were classified as squamous cell carcinoma, 29 (13.6%) as adenocarcinoma. For tumor grade, the majority were higher-grade: only 12 (5.6%) were classified as G1; 110 (51.4%) were G2, and 92 (43%) were G3.
The median follow-up period was 32 months. During the follow-up period, 100 (46.7%) of the patients had disease recurrence, with a median time to recurrence of 10 months. The pelvis was the primary site of recurrence in 54 (54%) cases; recurrence location was distant in 47 cases (47%).
During follow-up, 57 of the 214 patients (26.6%) died; the median time to death was 27 months, and death was attributed to cervical cancer in 50 (87.7%) cases.
Cystoscopy was performed preoperatively in all 103 patients from Center A; at Center B, cystoscopy was performed on only 26 patients, for whom bladder wall infiltration appeared in the original MRI report or was clinically suspected. The remaining patients underwent urine cytology.
Of these 129 patients, endoscopic biopsy was positive for bladder mucosa infiltration in nine (7%) and negative in 120 (93%). All 85 cases in which urine cytology was performed were negative for bladder mucosa infiltration.
However, on MRI, while all nine patients with bladder mucosa infiltration on cystoscopy were shown to have bladder wall invasion, the other 35 of the 44 (79.5%) patients with MRI-defined bladder wall invasion showed no mucosal infiltration on cystoscopy.
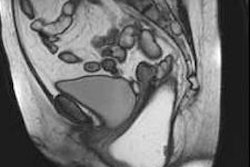
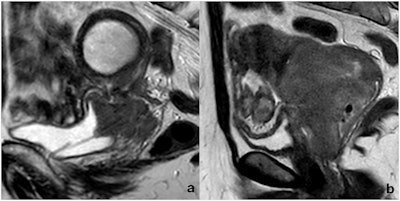 Two cases of MRI-defined bladder wall invasion on sagittal FSE T2-weighted images. (a) A complete loss of neoplasm-bladder cleavage plan, a massive bladder wall thickening with intermediate signal intensity, as well as endoluminal tumor growth, is appreciable; a DJ catheter was placed because of hydronephrosis. (b) An incomplete loss of neoplasm-bladder cleavage plan and a discrete bladder wall thickening with intermediate signal intensity is appreciable, but no endoluminal tumor growth can be observed. The first case was positive at cystoscopy, whereas the second one was negative. Both patients underwent local tumor recurrence (13 and 19 months after chemoradiation, respectively), and both died (25 and 36 months after initial diagnosis, respectively).Bonatti et al; European Radiology
Two cases of MRI-defined bladder wall invasion on sagittal FSE T2-weighted images. (a) A complete loss of neoplasm-bladder cleavage plan, a massive bladder wall thickening with intermediate signal intensity, as well as endoluminal tumor growth, is appreciable; a DJ catheter was placed because of hydronephrosis. (b) An incomplete loss of neoplasm-bladder cleavage plan and a discrete bladder wall thickening with intermediate signal intensity is appreciable, but no endoluminal tumor growth can be observed. The first case was positive at cystoscopy, whereas the second one was negative. Both patients underwent local tumor recurrence (13 and 19 months after chemoradiation, respectively), and both died (25 and 36 months after initial diagnosis, respectively).Bonatti et al; European Radiology
Furthermore, the study team found that the patients with MRI-defined bladder wall invasion had a significantly higher risk of mortality compared with those without (hazard ratio, 3.74; 95% confidence interval: 1.94-7.24; p = 0.005). There was no statistically significant difference in survival rates between the nine patients with both MRI-defined bladder wall invasion and cystoscopy-defined bladder mucosa infiltration and the 37 patients with MRI-defined bladder wall invasion and no cystoscopy findings, the researchers added.
The findings show not only that MRI is effective in ruling out bladder mucosa infiltration in cervical cancer patients, but also that “MRI-defined bladder wall invasion has a strong prognostic impact on both disease-free and overall survival, much stronger than that of cystoscopy-defined bladder mucosa infiltration.” This suggests, in turn, that MRI could be used as the “gold standard” for assessing bladder involvement with cervical cancer.
Read the study here.