Emerging 3D MR segmentation techniques make it feasible to quantify tumor burden and provide a quick visual assessment of lesion distribution throughout the knee, but the process is time-consuming and operator-dependent, and more automation is needed, Dutch researchers have found.
Orthopedic surgeons and radiologists at Leiden University Medical Centre performed a first step towards objective volumetric quantification of diffuse-type tenosynovial giant cell tumor (D-TGCT) by segmenting 3D tumor volume in 40 treatment-naïve patients with D-TGCT. They published their preliminary findings in an article posted on 1 February by Insights into Imaging.
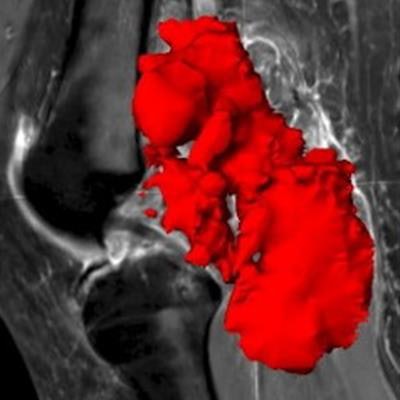
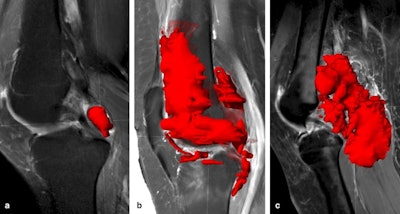 Examples of volumetric segmentation in three different patients. Volumetric segmentations of D-TGCT performed with Brainlab software on sagittal T1 SPIR-weighted sequences post gadolinium. (A) tumor is segmented in the posterior cruciate ligament (PCL) recess (volume shown in red). Volume = 3.8 cm3. (B) Tumor segmentation in anterior, middle, and posterior compartments. Volume = 86.2 cm3. (C) Tumor segmentation of a case with marked posterior disease, present in the PCL recess, subgastrocnemius synovial recesses, Baker's cyst, and extending extra-articular in the popliteal fossa. Volume = 91.9 cm3. Figures courtesy of Dr. Geert Spierenburg, Dr. Kirsten van Langevelde, et al and Insights into Imaging.
Examples of volumetric segmentation in three different patients. Volumetric segmentations of D-TGCT performed with Brainlab software on sagittal T1 SPIR-weighted sequences post gadolinium. (A) tumor is segmented in the posterior cruciate ligament (PCL) recess (volume shown in red). Volume = 3.8 cm3. (B) Tumor segmentation in anterior, middle, and posterior compartments. Volume = 86.2 cm3. (C) Tumor segmentation of a case with marked posterior disease, present in the PCL recess, subgastrocnemius synovial recesses, Baker's cyst, and extending extra-articular in the popliteal fossa. Volume = 91.9 cm3. Figures courtesy of Dr. Geert Spierenburg, Dr. Kirsten van Langevelde, et al and Insights into Imaging."3D segmentation is not part of our standard diagnostics -- this was done as a pilot study, in a research setting," first author Geert Spierenburg (trainee orthopedic surgeon) and senior author Dr. Kirsten van Langevelde (musculoskeletal radiologist) told AuntMinnieEurope.com in an email. "We find that using RECIST for tumor response assessment is just not a useful method for these diffusely growing synovial tumors."
Volumetric quantification techniques integrated with deep learning methods may help measure tumor change, but developing such an automated quantification method is challenging due to irregular growth and heterogeneous signal intensity of TGCTs, they explained.
For 3D segmentation, the researchers used gadolinium-enhanced sagittal T1-weighted spectral inversion recovery (SPIR) and an axial T2 DIXON (water only) scan. Measuring tumor volume was done in Brainlab Elements, an application that is commonly used for preoperative planning of bone and soft-tissue tumors.
Usefulness of MRI
MRI is the modality of choice to diagnose TGCTs and discriminate between subtypes, and it can also provide a preoperative map before synovectomy, the mainstay of treatment, the authors noted.
"Since the arrival of colony-stimulating factor 1-receptor inhibitors, a novel systemic therapy for D-TGCT patients with relapsed or inoperable disease, MRI is key in assessing treatment response," they noted. "As recurrence after treatment of D-TGCT occurs more often than in lateral TGCT, follow-up imaging plays an important role in D-TGCT."
Reading follow-up MRIs of these diffuse synovial tumors may be a daunting task, they continued, and it's important to provide a systematic approach to assess the knee synovial recesses, highlight D-TGCT imaging findings, and combine these into a structured report. In addition, it is important to bear in mind differential diagnoses mimicking D-TGCT, potential pitfalls, and evaluation of tumor response following systemic therapies.
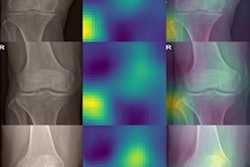
 55-year-old man with differential diagnosis of gout in the knee. (A) Lateral radiograph demonstrates marked pre-patellar soft-tissue swelling containing increased density and several ill-defined calcifications (arrow). (B) Sagittal T1 shows a prepatellar, low signal intensity oval-shaped soft tissue mass and a subchondral cyst in the patella. (C) Axial T2-weighted fat-suppressed MRI confirms the prepatellar, low signal intensity mass invading the quadriceps tendon (arrows) and shows joint effusion containing multiple small synovial proliferations in the suprapatellar recess (asterisk). Aspiration of joint fluid with crystals confirmed the diagnosis of gout. (D) Axial T2-weighted fat-suppressed MRI demonstrates low signal intensity soft tissue lesions in keeping with gout tophi deep to the collateral ligaments, causing erosion of the medial and lateral femoral condyles (arrows).
55-year-old man with differential diagnosis of gout in the knee. (A) Lateral radiograph demonstrates marked pre-patellar soft-tissue swelling containing increased density and several ill-defined calcifications (arrow). (B) Sagittal T1 shows a prepatellar, low signal intensity oval-shaped soft tissue mass and a subchondral cyst in the patella. (C) Axial T2-weighted fat-suppressed MRI confirms the prepatellar, low signal intensity mass invading the quadriceps tendon (arrows) and shows joint effusion containing multiple small synovial proliferations in the suprapatellar recess (asterisk). Aspiration of joint fluid with crystals confirmed the diagnosis of gout. (D) Axial T2-weighted fat-suppressed MRI demonstrates low signal intensity soft tissue lesions in keeping with gout tophi deep to the collateral ligaments, causing erosion of the medial and lateral femoral condyles (arrows)."We see around 50 new patients each year. In addition, we follow up patients regularly, especially the diffuse-type TGCTs," Spierenburg and van Langevelde pointed out. "For this tumor entity, contrast-enhanced MRI scans have been part of the standard of care for around two decades in our center."
At present, the Leiden group does not have any active studies to develop automatic 3D segmentation for TGCTs, although they are keen to expand on this concept.
"During our pilot study, we had a dedicated radiology fellow working with us (Dr. Carlos Suevos Ballesteros from the Department of Radiology, Hospital Universitario Ramón y Cajal, Madrid) and together with him we found that it was very time-consuming to segment the tumors manually," they noted. "And because of TGCT's heterogeneous distribution and size within the knee joint, we believe that it requires a larger number of cases to train machine learning, i.e., AI-driven 3D segmentation."
Incidental findings
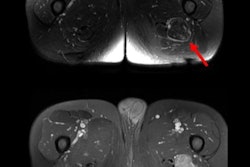
In their email to AuntMinnieEurope.com, Spierenburg and van Langevelde also commented on the TGCT case published on 26 January 2023 in the Journal of Nuclear Medicine.
"We do sometimes come across TGCT as an incidental finding, for example in the knee or around the wrist on [F-18 FDG-PET-CT] scans or on whole body MRI scans," they stated. "However, these cases are asymptomatic localized-TGCTs, which can be highly FDG-avid. We have never come across a case of incidental diffuse-type TGCT because these tumors are mostly more extensive and symptomatic."
Based on the images provided in this case report, this case appears to be a localized-type TGCT, possibly related to a hamstring tendon, they added. "In addition, there is an entity called 'giant cell tumor of soft tissue,' which is a totally different entity in the WHO book on soft tissue and bone tumors, and sometimes causes confusion with the terminology of TGCT. This may also present as a painless growing mass in the extremities."