While mammography is the only proven modality to effectively detect cancer, its sensitivity declines with increasing density of breast tissue. So how can radiologists prevent women with dense breasts from slipping through the screening net?
Researchers from Austria have shown that supplemental ultrasound improves cancer detection in the screening of women with an average risk of breast cancer while maintaining recall and biopsy rates at an acceptable level. The team from the University for Health Sciences, Medical Informatics and Technology (UMIT), in Hall in Tirol published their findings in the April 2018 issue of the European Journal of Radiology.
"The most important finding of our study was that the increase in sensitivity due to additive ultrasound observed in clinical studies with a limited number of cases could be confirmed in a population-based screening program, whereas the negative effects, namely increased false-positive rates and biopsy rates were much lower than expected," lead study author Dr. Wolfgang Buchberger, professor of radiology and consultant at Innsbruck University Hospital, told AuntMinnieEurope.com. "In our series, only 1.7% of women screened were recalled for further assessment and 0.9% underwent biopsy, which is lower than in most European screening programs with mammography only."
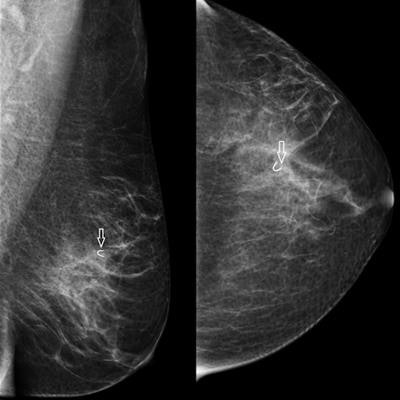
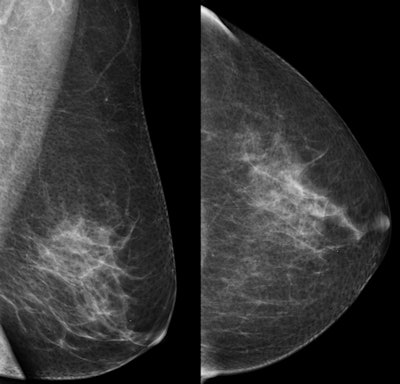 Top: Oblique and craniocaudal screening mammograms of a 51-year-old woman show no abnormality. Below: Ultrasound shows a 7-mm ductal invasive carcinoma (calipers). Bottom: Oblique and craniocaudal mammograms after ultrasound-guided core needle biopsy show clipmarker at biopsy site (arrow). All images courtesy of Dr. Wolfgang Buchberger.
Top: Oblique and craniocaudal screening mammograms of a 51-year-old woman show no abnormality. Below: Ultrasound shows a 7-mm ductal invasive carcinoma (calipers). Bottom: Oblique and craniocaudal mammograms after ultrasound-guided core needle biopsy show clipmarker at biopsy site (arrow). All images courtesy of Dr. Wolfgang Buchberger.Data from past smaller studies on women with a higher risk of cancer show that adding handheld ultrasound to mammography for women with dense breasts increases cancer detection rates at the expense of lower specificity and lower positive predictive values, the authors noted (Eur J Radiol, April 2018, Vol. 101, pp. 24-29). Therefore, the team wanted to study how the addition of ultrasound, with its improved technology and reporting standards, could have an impact on mammography screening for a larger sample of women with an average breast cancer risk.
Study group
The researchers retrospectively looked at 66,680 screening exams using mammography and bilateral ultrasound from the Tyrolean breast cancer screening program that were performed between June 2008 and May 2010. Of these, 31,066 (46.6%) women were 40 to 49 years old, 21,609 (32.4%) were 50 to 59 years old, and 14,013 (21.0%) were 60 to 69 years old. In terms of breast tissue, 31,918 women (47.9%) had extremely dense or heterogeneously dense breasts, and this percentage was 54.4% in woman ages 40 to 49, 45.6% for those ages 40 to 49, and 36.9% for women ages 60 to 69.
The researchers used histological results and follow-up at one year as the reference standard for sensitivity. For main outcome measures, they used cancer detection rate, sensitivity, recall rate, biopsy rate, and positive predictive value of biopsy for combined screening with mammography plus ultrasound versus mammography alone.
Clear results
The overall sensitivity rates for mammography only and mammography plus ultrasound for women with dense and nondense breasts are shown in the table below.
| Sensitivity rates for dense & nondense breasts | ||
| Total 66,680 women | Sensitivity for dense breasts | Sensitivity for nondense breasts |
| Mammography alone | 61.5% | 86.6% |
| Mammography plus ultrasound | 81.3% | 95.0% |
The absolute gain in sensitivity was 19.8% in women with dense breasts and 8.4% in women with nondense breasts.
Overall sensitivity of screening was 78.5% for mammography alone and 90.6% for combined screening with mammography and ultrasound. During a follow-up period of 12 months, 28 interval cancers were identified equivalent to an interval cancer rate of 0.42 missed cancers per 1,000 screens. According to the European guidelines, the interval cancer rate within 11 months after the screening examination should not exceed 30% of the background incidence rate in the absence of screening, the authors noted. In the current study, in relation to a background incidence rate of 1.78 cancers per 1,000 women, the proportional incidence for first-year interval cancers was only 23.7%.
Adjunctive ultrasound increased the recall rate from 10.5 to 16.5 per 1,000 women screened, and it increased the biopsy rate from 6.3 to 9.3 per 1,000 women screened. The positive predictive value of biopsy was 55.5% (95% confidence interval [CI]: 50.6% to 60.3%) for mammography alone and 43.3 (95% CI: 39.4% to 47.3%) for combined mammography plus ultrasound.
Additional cancers
Based on BI-RADS assessments, 234 cancers (210 invasive carcinomas and 24 ductal carcinoma in situ [DCIS]) were identified on mammography, and 36 cancers (33 invasive cancers and three DCIS) were additionally detected by ultrasound. The ultrasound-detected cancers were not different in size and stage from mammographically detected cancers. Of the 36 cancers detected by ultrasound only, 19 (52.8%) occurred in women with heterogeneously dense or extremely dense breasts. The proportion of ultrasound-only detected cancers was 24.4% (19/78) in women with dense breasts and 8.9% (17/192) in women with nondense breasts.
Changing practice
The main reason why supplemental ultrasound has not yet been implemented in population-based screening for women at normal risk of cancer is the comparably low positive predictive value with regard to detecting additional malignancies seen in previous studies, according to the authors.
For example, in the institute's previous study of 8,970 women, ultrasound detected 32 cancers and 330 benign lesions; therefore, 9 out of 10 ultrasound-detected lesions were benign.
 Dr. Wolfgang Buchberger from Innsbruck University Hospital.
Dr. Wolfgang Buchberger from Innsbruck University Hospital.However, ultrasound technology has improved significantly in recent years, and the introduction of the ultrasound BI-RADS lexicon has led to the standardization of diagnosis and reporting, Buchberger noted.
"The team expected that the rate of false-positive findings would decrease compared to the results from 10 to 15 years ago when most ultrasound screening studies were published, and this hypothesis was correct," he said.
The authors also pointed to the multicenter ACRIN 6666 trial, in which the positive predictive value of biopsy recommendations after full diagnostic workup was 22.6% for mammography, 8.9% for ultrasound, and 11.2% for combined mammography and ultrasound.
"In our study, the positive predictive value of biopsies resulting from combined mammography plus ultrasound was significantly higher, namely 37.7% in women with dense breasts and 46.2% in women with nondense breasts," wrote the authors, adding that the overall performance characteristics of combined screening with mammography and ultrasound were within accepted ranges.
In addition, they noted that a recent overview of the European mammography screening programs showed the overall rates of further assessment for initial and subsequent screening tests to be 9.3% and 4.0%, the overall rates of needle biopsy 2.2% and 1.1%, and the overall rates of surgical interventions 1.0% and 0.7%, respectively. In the current study, only 1.7% of women screened were recalled for further assessment and 0.9% underwent biopsy.
One reason for such favorable results may be the high level of experience of participating radiologists, the authors stated.
However, they warned that unlike in most European screening programs, double reading of mammograms was not performed and that it was possible that single reading of mammograms led to a slight overestimation of the benefit of adjunctive ultrasound.
That said, they suggested that because most cancers additionally detected by ultrasound were invasive, small in size, and node-negative, increasing detection of such cancers should correlate with mortality reduction. Therefore, prospective randomized trials were needed to compare the clinical outcomes of different screening approaches.
Supplemental ultrasound screening is feasible in mass screening, and the adverse effects in terms of recall rates and biopsy rates are comparable with those reported for population-based screening programs using mammography only, Buchberger explained.
"Currently, additional ultrasound screening in women with dense breasts is being tested in the Austrian national breast cancer screening program. If these results are confirmed in further screening studies, a change of breast cancer screening policies may be considered," he said.