Conebeam breast CT (CBBCT) has superior diagnostic performance than that of mammography in small studies, according to research published on 8 January in the European Journal of Radiology.
A team led by Lingcong Yang from Southern Medical University in Guangzhou, China, reported in its meta-analysis that CBBCT has significantly higher sensitivity than mammography along with comparable specificity.
“However, the results of both CBBCT and mammography are based on studies with small sample sizes,” the Yang team wrote.
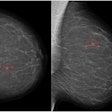
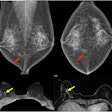
CBBCT in recent years has garnered interest among radiologists as another way to diagnose breast cancer. The modality provides isotropic 3D images, which the researchers highlighted eliminates the need for breast compression. CBBCT uses a cone-shaped x-ray beam to acquire multiple 2D images from various angles around the breast. From there, it reconstructs these images into a 3D model.
Yang and colleagues noted that CBBCT’s diagnostic performance has not been compared with that of standard mammography in systematic reviews. They added to the literature by evaluating eight research articles that directly compared the diagnostic value of both modalities for primary breast cancer.
In total, the studies included 847 participants. They were published between 2015 and 2022. Of the studies, six were retrospective and two were prospective. Additionally, seven studies were based on lesion analysis while the remaining one focused on patient analysis.
CBBCT overall had a higher area under the curve (AUC) value than that of mammography, owing to higher sensitivity and similar specificity.
| Comparison between CBBCT, mammography | ||
|---|---|---|
| Measure | Mammography | CBBCT |
| AUC | 0.83 | 0.93 |
| Sensitivity | 77% | 92% |
| Specificity | 75% | 79% |
The researchers also performed a Z-test to analyze the differences in summary diagnostic performance between the two modalities. They reported that the summary sensitivity and AUC of CBBCT were significantly higher than that of mammography (p < 0.001 for both).
The study authors highlighted that CBBCT’s performance owes to the modality’s ability to capture the size, shape, and spatial relationship of breast lesions with the surrounding tissues more effectively.
However, they called for future research to use larger sample sizes to gather more robust results for better applications in clinical practice.
“In addition, careful consideration of the advantages and disadvantages of CBBCT and mammography is essential for clinical decision-making,” they concluded. “While CBBCT demonstrates better sensitivity and overall diagnostic performance, it is important to acknowledge its potential drawbacks, including higher costs and lower accessibility when compared to mammography."
The study can be found in its entirety here.