Digital breast tomosynthesis (DBT)-guided biopsy offers a viable option for lesions detected by MRI and contrast-enhanced mammography (CEM), especially for nonmass enhancements that are not identified on second-look ultrasound, Spanish researchers have found.
In their study presented as a poster at RSNA 2023, Dr. César Urtasun Iriarte and colleagues from the department of radiology at Navarra University Hospital in Pamplona, noted that their aims were to emphasize the need to correlate MRI and CEM findings with DBT, to show the advantages of DBT-guided biopsies compared to MRI-guided biopsies, and to consider DBT-guided biopsies as an alternative for CEM-detected lesions.
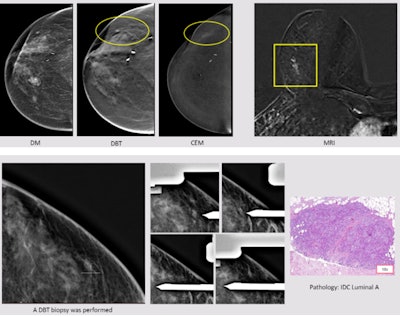 A 55-year-old woman with a previous left mastectomy and right tumorectomy in 2010 (ductal carcinoma in situ, DCIS) had a recent diagnosis of positive right axillary lymph node (metastases from invasive ductal carcinoma, IDC). Digital mammography, DBT, and ultrasound were normal, but CEM showed a nonmass enhancement in the inferior outer quadrant (circle). On DBT, a subtle distortion was found in correlation with CEM/MRI (square). A DBT-guided biopsy was performed, leading to a diagnosis of IDC luminal A. All images courtesy of Dr. César Urtasun Iriarte et al and presented at RSNA 2023.
A 55-year-old woman with a previous left mastectomy and right tumorectomy in 2010 (ductal carcinoma in situ, DCIS) had a recent diagnosis of positive right axillary lymph node (metastases from invasive ductal carcinoma, IDC). Digital mammography, DBT, and ultrasound were normal, but CEM showed a nonmass enhancement in the inferior outer quadrant (circle). On DBT, a subtle distortion was found in correlation with CEM/MRI (square). A DBT-guided biopsy was performed, leading to a diagnosis of IDC luminal A. All images courtesy of Dr. César Urtasun Iriarte et al and presented at RSNA 2023.
Both MRI and CEM are morphofunctional imaging techniques based on neoangiogenesis (the development of new blood vessels from a pre-existing vasculature). These techniques are more sensitive than pure morphological techniques used to diagnose breast cancer, such as digital mammography or DBT, they explained.
Second-look ultrasound is the technique of choice to evaluate mass enhancements, yet the assessment of nonmass enhancements is more challenging. Although ultrasound plays an important role, in many cases, it is inconclusive. DBT correlation is very important, specifically using the craniocaudal (CC) view. This view is easy to compare anatomical structures with both MRI (axial) and CEM.
“The key is to use the CC view/axial MRI view for correlation,” they emphasized.
DBT-guided biopsies offer significant advantages over MRI or CEM-guided biopsies. They are less time-consuming; MRI-guided biopsies can take longer due to the need for multiple scans and adjustments. Also, a DBT-guided biopsy is generally more comfortable than an MRI-guided biopsy because it is a less invasive procedure.
“DBT-guided biopsy makes it easier to identify certain findings such as architectural distortion and has improved margin analysis compared to MRI-guided biopsy,” the authors wrote. “DBT-guided biopsy is cheaper and more widely available and accessible, making it a more cost-effective option for patients and healthcare providers.”
Not all the vendors have dedicated units to perform CEM guided biopsies, they continued. “Once the lesion is located with DBT, the performance of the biopsy is easy. Usually 10G vacuum-assisted biopsy devices are used.”
On the flip side, DBT-guided biopsies may be less accurate for certain types of lesions, such as those that are particularly small or noncalcified. Also, they may have lower sensitivity and performance rates in certain areas such as the axilla, and even though DBT-guided biopsies require fewer exposures and therefore a smaller total radiation dose compared to digital mammography-guided biopsies, MRI-guided biopsies stand out as the zero-radiation option, according to the authors.
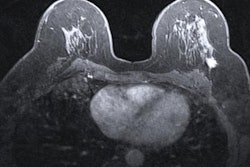
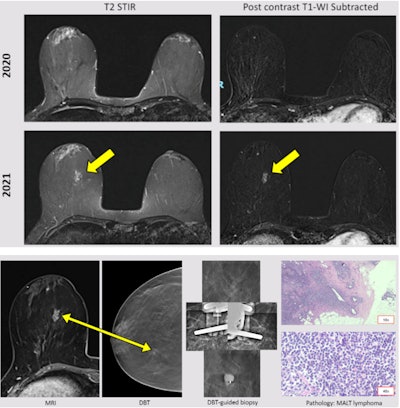 A 48-year-old woman diagnosed with Hodgkin lymphoma in 1999 and treated with chemotherapy and radiotherapy. Ultrasound was normal. MRI follow-up showed a new nonmass enhancement in the right breast (yellow arrow). DBT showed a focal asymmetry. Good correlation with the MRI finding. A DBT-guided vacuum-assisted biopsy was performed, leading to a diagnosis of mucosa associated lymphoid tissue (MALT) lymphoma.
A 48-year-old woman diagnosed with Hodgkin lymphoma in 1999 and treated with chemotherapy and radiotherapy. Ultrasound was normal. MRI follow-up showed a new nonmass enhancement in the right breast (yellow arrow). DBT showed a focal asymmetry. Good correlation with the MRI finding. A DBT-guided vacuum-assisted biopsy was performed, leading to a diagnosis of mucosa associated lymphoid tissue (MALT) lymphoma.
DBT images are used to locate the suspicious area in the breast -- a posterior lesion requires upright positioning, while anxiety and/or interior lesion require prone positioning. Patients should be asked to remove any clothing or jewelry from the waist up and are given a gown to wear during the exam, and the area around the biopsy site is numbed with local anesthetic.
After the biopsy, the patient is given a pressure bandage to wear over the biopsy site. She should avoid showering or bathing for 24 hours after the biopsy and should not participate in strenuous activities for 48 hours, they continued.
Editor’s Note: The coauthors of this exhibit were M. Barrio Piqueras, C. Mbongo, M. Jiménez, A. Elizalde, and L. Pina.