MRI defecography (MRD) can provide more complete information and limit challenges that make pelvic floor dysfunction (PFD) difficult to diagnose, researchers have found.
In an article on 28 January in the European Journal of Radiology, a University of Palermo (Italy) team headed by Dr. Rosa Alba Pugliesi of the Department of Biomedicine, Neuroscience and Advanced Diagnostics, delineated the MRD approach in the diagnosis of PFD.
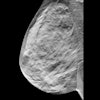
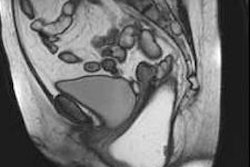
 Normal female pelvic floor anatomy. (A): Coronal T2-weighted MR defecography highlighting the levator ani complex and both internal and external anal sphincters. (B) Axial T2-weighted image depicts the urethral support structures: periurethral ligaments from the puborectalis, paraurethral ligaments (arrowheads) from the urethral wall, and pubourethral ligaments from the pubic bone to the urethra. The vagina (V) shows a typical H-shaped configuration. Ps = pubic symphysis, R = rectum, U = urethra, IS: internal anal sphincter, ES: external anal sphincter.Pugliesi et al; EJR
Normal female pelvic floor anatomy. (A): Coronal T2-weighted MR defecography highlighting the levator ani complex and both internal and external anal sphincters. (B) Axial T2-weighted image depicts the urethral support structures: periurethral ligaments from the puborectalis, paraurethral ligaments (arrowheads) from the urethral wall, and pubourethral ligaments from the pubic bone to the urethra. The vagina (V) shows a typical H-shaped configuration. Ps = pubic symphysis, R = rectum, U = urethra, IS: internal anal sphincter, ES: external anal sphincter.Pugliesi et al; EJR
PFD, a spectrum of disorders affecting approximately 50% of women in Western nations, can be difficult to diagnose due to nonspecific symptoms and exams that often underestimate the extent of multicompartmental disease and may not reproduce the patient’s symptoms, the authors said.
MRD is a noninvasive imaging technique that provides high-resolution imaging of the pelvic-floor anatomy in different functional states. It is particularly useful, Pugliesi and colleagues wrote, for complex or postoperative cases, as it enables detection of postsurgical complications and findings such as cystoceles, rectoceles, enteroceles, uterine or vaginal prolapse, and intussusception.
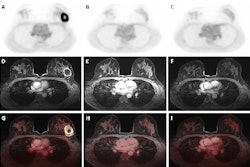
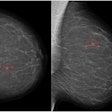
 Real-time evaluation of PFD Using T2-weighted interactive single shot sequence (SSFSE) in dynamic MR defecography. Dynamic MR defecography using T2-weighted SSFSE sequence shows pelvic floor anatomy at rest (A), during squeezing (B), and defecation (C). Progressive descent of pelvic organs suggests pelvic floor dysfunction. B: bladder, Ps = pubic symphysis, R: rectum, Ut: Uterus.Pugliesi et al; EJR
Real-time evaluation of PFD Using T2-weighted interactive single shot sequence (SSFSE) in dynamic MR defecography. Dynamic MR defecography using T2-weighted SSFSE sequence shows pelvic floor anatomy at rest (A), during squeezing (B), and defecation (C). Progressive descent of pelvic organs suggests pelvic floor dysfunction. B: bladder, Ps = pubic symphysis, R: rectum, Ut: Uterus.Pugliesi et al; EJR
MRD also highlights stabilizing structures in the pelvis, such as the urogenital diaphragm, endopelvic fascia, and levator ani complex, the researchers added.
To provide the most comprehensive evaluation of functional issues, the team highlighted the need for full imaging of the defecation process, as it captures a fuller extent of pelvic organ descent, they wrote.
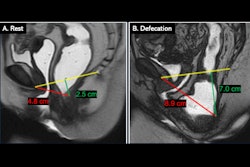
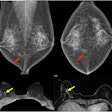
 Anterior rectocele with pelvic floor descent during defecation phase, consistent with pelvic floor dyssynergia and structural pelvic organ prolapse. Midsagittal fast field echo (BFFE) images during the squeezing phase (left) and defecation phase (right) demonstrate anorectal angle dynamics. During defecation, note the presence of an anterior rectocele (*), protruding beyond the H-line, indicating pelvic floor dysfunction. Pubic symphysis (Ps), rectum (R), bladder (B).Pugliesi et al; EJR
Anterior rectocele with pelvic floor descent during defecation phase, consistent with pelvic floor dyssynergia and structural pelvic organ prolapse. Midsagittal fast field echo (BFFE) images during the squeezing phase (left) and defecation phase (right) demonstrate anorectal angle dynamics. During defecation, note the presence of an anterior rectocele (*), protruding beyond the H-line, indicating pelvic floor dysfunction. Pubic symphysis (Ps), rectum (R), bladder (B).Pugliesi et al; EJR
While fluoroscopy and ultrasound are both useful modalities for diagnosing PFD, the authors noted that each has its restrictions. Fluoroscopy offers only limited soft-tissue contrast, cannot simultaneously evaluate all three pelvic-floor compartments, and involves the use of radiation. Ultrasound, while useful for assessing the anterior compartment, has limited utility for full evaluation of the pelvic floor. MRD has none of the shortcomings listed for either approach: It provides high soft-tissue contrast without radiation and can dynamically evaluate all compartments.
According to Pugliesi and colleagues, pelvic organ support in PFD is commonly assessed with the Pelvic Organ Prolapse Quantification (POP-Q) system, which evaluates prolapse using anatomical reference points in three compartments: anterior, apical (middle), and posterior. To facilitate diagnosis, guide surgical planning, and enable postsurgical assessment, POP-Q includes a staging classification from Stage 0 (no prolapse) to Stage 4 (essentially complete vaginal eversion).
 Sagittal T2-weighted MRD image at maximal pelvic floor contraction (squeeze). The pubococcygeal line (PCL) serves as a reference line extending from the inferior border of the pubic symphysis to the last coccygeal joint. The H line represents the anteroposterior dimension of the levator hiatus, while the M line measures the perpendicular descent of the levator plate relative to the PCL. The midpubic line (MPL) provides an additional reference for anterior-posterior alignment. Identifiable pelvic structures include the pubic symphysis (Ps), rectum (R), and bladder (B).Pugliesi et al; EJR
Sagittal T2-weighted MRD image at maximal pelvic floor contraction (squeeze). The pubococcygeal line (PCL) serves as a reference line extending from the inferior border of the pubic symphysis to the last coccygeal joint. The H line represents the anteroposterior dimension of the levator hiatus, while the M line measures the perpendicular descent of the levator plate relative to the PCL. The midpubic line (MPL) provides an additional reference for anterior-posterior alignment. Identifiable pelvic structures include the pubic symphysis (Ps), rectum (R), and bladder (B).Pugliesi et al; EJR
However, the authors explained that MRD goes beyond the traditional three-compartment descriptors in that it emphasizes the integrated functional anatomy, as PFD affects multiple systems, and allows for evaluation of muscular integrity -- an element increasingly noted as important in the diagnosis and management of PFD.
While acknowledging limitations of the POP-Q system, the researchers wrote that it “remains the clinical standard and is commonly correlated with MRI measurements, as shown by studies reporting variable correlation between POP-Q and MRD across compartments.” They suggested that a combination of approaches -- using the POP-Q staging system with MRD grading -- will provide more comprehensive information for diagnosing PFD and guiding surgical decisions by providing correlated data.
Additionally, they stated that MRD, with its emphasis on linking the structural and functional, establishes a consistent, reproducible framework in evaluating and monitoring PFD and its potential complications over time.
However, MRD is not completely without drawbacks, Pugliesi and colleagues noted. Interpretation of MRD may be affected by the operator’s experience level, technical variance, and patient positioning. The supine positioning of MRI (as compared to sitting or upright imaging used in conventional exams) may result in underestimation of prolapse; this is one of the reasons the authors have recommended an approach combining MRD with clinical exam using the POP-Q staging system.
MRD is also not as effective for evaluating neuromuscular function as anorectal manometry or electromyography, which provide findings on pelvic floor and sphincter function beyond what imaging is capable of. In addition, the high cost and limited availability of MR imaging may be significant barriers to clinicians using the MRD approach.
Read the article, which includes detailed information on the affected pelvic anatomy and MRD protocols, here.