Patients with Li-Fraumeni syndrome (LFS), a rare genetic condition in which the risk for developing certain types of cancer is exceptionally elevated, require regular surveillance for early cancer detection. Currently, the recommendation for patients with LFS is annual whole-body MRI (WB-MRI); however, there is no standardized protocol established for the procedure.
In an article published by European Radiology on 21 October, Dr. Myriam Keymling from the radiology department of the German Cancer Research Center (DKFZ) in Heidelberg and colleagues aimed to establish an optimized protocol of WB-MRI for annual LFS surveillance.
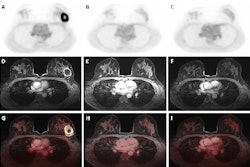
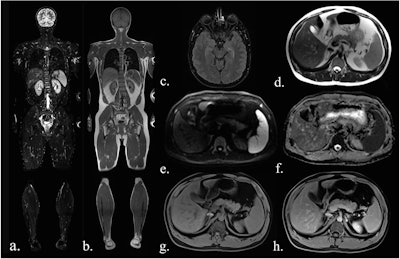 Sequences included in the study MRI protocol: (a) coronal TIRM (turbo inversion recovery magnitude) sequence, (b) coronal T1-weighted sequence, (c) axial FLAIR (fluid-attenuated inversion recovery) sequence (head only), (d) axial T2-weighted fast spin-echo sequence (HASTE), (e) axial diffusion-weighted imaging (b-value 900), (f) an axial ADC map, (g) axial T1-Dixon water-only images before contrast agent, and (h) after administration of contrast agent.All figures courtesy of Dr. Myriam Keymling et al and European Radiology
Sequences included in the study MRI protocol: (a) coronal TIRM (turbo inversion recovery magnitude) sequence, (b) coronal T1-weighted sequence, (c) axial FLAIR (fluid-attenuated inversion recovery) sequence (head only), (d) axial T2-weighted fast spin-echo sequence (HASTE), (e) axial diffusion-weighted imaging (b-value 900), (f) an axial ADC map, (g) axial T1-Dixon water-only images before contrast agent, and (h) after administration of contrast agent.All figures courtesy of Dr. Myriam Keymling et al and European Radiology
In the prospective study, 113 participants with LFS underwent a total of 189 WB-MRI exams over 30 months at the DKFZ and at Hannover Medical School. The 189 exams consisted of 113 baseline exams, with 69 follow-up exams after one year and seven follow-up exams after two years.
Combinations of sequences were assessed in order to determine the optimal protocols. The analysis included turbo-spin echo (TSE) T1-weighted and inversion-recovery T2-weighted (TIRM) images of the whole body in coronal orientation, and T2-weighted (HASTE), diffusion-weighted (DWI), and T1-weighted DIXON images (pre- and postcontrast agent administration) from head to thighs in axial orientation. An additional fluid-attenuated inversion recovery (FLAIR) sequence was used for the skull only.
FLAIR and DWI sequences, alone and in combination, demonstrated the best results for all lesions (benign, ambiguous, malignant). DWI achieved the highest score for imaging malignant lesions in the entire body (86% of lesions categorized as “easily detectable”), while FLAIR had the best results for lesions of the head (100% of “easily detectable” lesions). DWI and FLAIR consistently demonstrated the highest ratings for malignant lesions of two-sequence combinations. The most effective three-sequence combination for all lesions was DWI and contrast-enhanced T1W with TIRM, according to the findings.
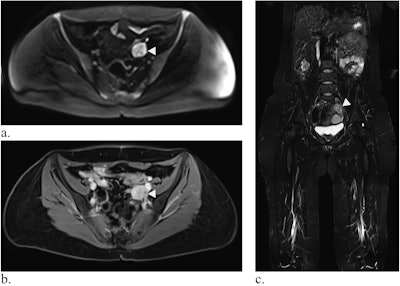 Whole-body MRI of a 39-year-old woman with LFS showing a mass in the small pelvis (white arrow) in diffusion-weighted imaging (a) and contrast-enhanced T1-weighted Dixon images (b, here: water-only image). In the coronal TIRM-sequence (c), the mass is visible, but difficult to differentiate from the intestine, emphasizing the value of diffusion-weighted imaging. Histology revealed a leiomyosarcoma.
Whole-body MRI of a 39-year-old woman with LFS showing a mass in the small pelvis (white arrow) in diffusion-weighted imaging (a) and contrast-enhanced T1-weighted Dixon images (b, here: water-only image). In the coronal TIRM-sequence (c), the mass is visible, but difficult to differentiate from the intestine, emphasizing the value of diffusion-weighted imaging. Histology revealed a leiomyosarcoma.
The WB-MRI protocol showed excellent overall sensitivity (90%) and specificity (83%) for detecting malignant lesions, thus “reaffirming the relevance of WB-MRI in recommendations for LFS surveillance.”
The best individual sequence overall was DWI, the team found. The combination of FLAIR (head) and DWI (head to thigh), and either HASTE or a contrast-enhanced T1-weighted DIXON sequence produced the best results: both combinations categorized all malignant lesions identified during the study period as “easily detectable” in at least one sequence, the authors wrote.
Of the additional exams triggered by WB-MRI, 94.4% identified lesions, 63.9% of which required therapy or close monitoring, while 1.1% led to unnecessary further investigation. If ultimately benign lesions requiring further investigation were considered false positives, they would bring the percentage of unnecessary investigations to 6.9% and the false-positive rate to 10.7% from 3.6%. However, the authors note that “[g]iven the increased risk of benign lesions progressing into malignancy in the context of LFS, additional workup of ultimately benign lesions was not classified as false positive.”
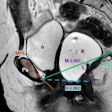
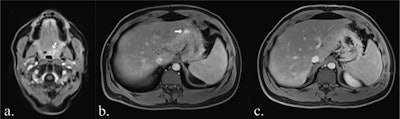 Examples of false-positive findings: Contrast-enhancement in the T1 Dixon water-only image of the pharyngeal wall (white arrow in a) was confirmed as regular hyperplastic pharyngeal tissue on biopsy. A focal contrast-enhancement of the gastric wall (white arrow in b) was no longer detectable on follow-up MRI (c) and was retrospectively deemed an artifact.
Examples of false-positive findings: Contrast-enhancement in the T1 Dixon water-only image of the pharyngeal wall (white arrow in a) was confirmed as regular hyperplastic pharyngeal tissue on biopsy. A focal contrast-enhancement of the gastric wall (white arrow in b) was no longer detectable on follow-up MRI (c) and was retrospectively deemed an artifact.
A consideration in designing the optimal protocol, according to Keymling and colleagues, is the duration of the sequences: a shorter protocol may “alleviate patient stress associated with prolonged durations of lying in the MRI scanner.” While the relatively long duration of the DWI sequence (24 minutes) is mentioned, the findings show it to be an essential sequence.
The combination of FLAIR, DWI, and HASTE would have a duration of 36.5 minutes; the FLAIR, DWI, and contrast-enhanced T1 combination is even shorter in duration at 32.5 minutes. However, use of contrast agent in the latter combination with potential for long-term retention may be a concern, they added.
The full European Radiology paper may be read here.