An initiative is underway in Belgium to improve the justification and appropriateness of radiology referrals by integrating evidence-based guidelines in the clinical workflow of referring physicians and radiologists.
Belgium performs the third largest number of CT scans in Europe per head of the population (see figure below). However, research such as the EU-Just CT study shows that clinical imaging guidelines and prescription search support (PSS) systems can provide essential tools to improve appropriateness, according to Nils Reynders-Frederix, secretary of the Belgian Medical Imaging Platform (BELMIP), which consists of the Federal Public Service (FPS) for Public Health, the National Institute for Health and Disability Insurance (RIZIV), the Federal Agency for Nuclear Control (FANC), and representatives of the sector.
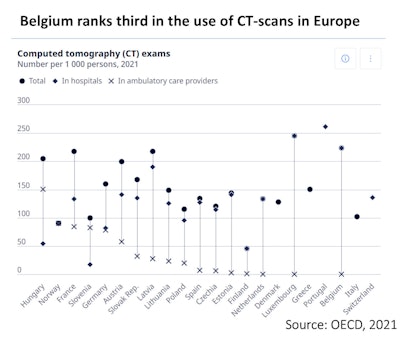 Organisation for Economic Co-operation and Development (OECD) indicators for CT exams, 2021. All figures courtesy of Reynders-Frederix et al and presented at EuroSafe 2025.
Organisation for Economic Co-operation and Development (OECD) indicators for CT exams, 2021. All figures courtesy of Reynders-Frederix et al and presented at EuroSafe 2025.
The plan is to create a nationwide digital referral prescription (DRP) for radiology and a government-funded PSS platform and then connect the platform to an external solution with evidence-based practice guidelines and integrate it with every Belgian hospital, GP practice, and radiology department, Reynders-Frederix and his colleagues explained in a EuroSafe 2025 e-poster.
Overall, their goal is to provide a positive clinical and educational environment, facilitate implementation and change management, impose mandatory use of prescription search support for radiology (PSSR) and data collection, and evaluate the impact at the level of referring physicians (appropriateness of referrals) and radiology departments (substitution and validation). Pilot projects are due to begin in 2026.
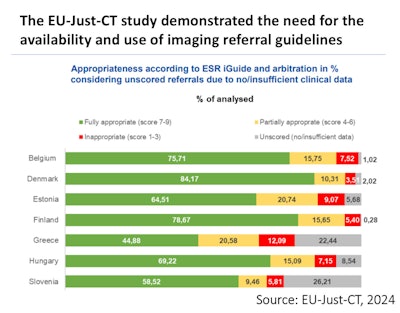 Appropriateness according to ESR iGuide and arbitration in percentages, considering unscored referrals due to no/insufficient clinical data.
Appropriateness according to ESR iGuide and arbitration in percentages, considering unscored referrals due to no/insufficient clinical data.
“Studies such as the EU-Just-CT study demonstrate the need for the availability and use of imaging referral guidelines,” the authors noted. “PSSR is a long-term project with the potential to improve quality, patient safety (radioprotection), justification, and appropriateness of medical imaging. It paves the way for further expansion into areas such as the appropriate use of antibiotics and clinical biology.”
The focus will be on patient care by providing innovative tools, backed up by support for both the referring physician and the radiologist to make optimal use of radiological examinations to ensure that the patient receives the most appropriate examination at the right time.
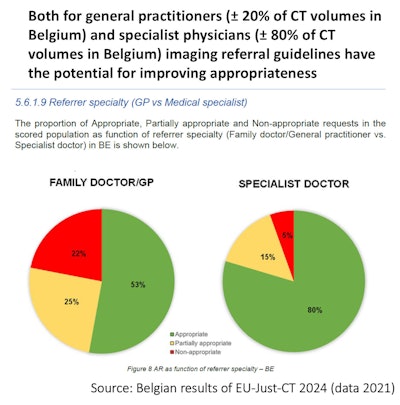 Belgian results of EU-Just-CT 2024 (data 2021).
Belgian results of EU-Just-CT 2024 (data 2021).
“The project has the potential to collect data for self-assessment or to monitor evolutions in justification,” they pointed out. “Healthcare stakeholders are at the forefront of this project and have been actively involved from the start. Extensive consultation and constructive cooperation between all stakeholders are crucial.”
Will the scheme succeed?
Long-term success depends on continuous updating of the guidelines and on feedback loops to refine the system based on real-world use, Prof. Erik Ranschaert, PhD, past president of the European Society of Medical Imaging Informatics (EuSoMII) and visiting professor at Ghent University in Belgium, told AuntMinnieEurope.
“While the goals remain valid and theoretically achievable, their success in practice will strongly depend on careful change management, IT resource allocation, and above all, a bottom-up engagement of referring physicians. Without this, even the most well-intentioned clinical decision support (CDS) system risks being underutilized,” he added.
The situation in the Netherlands and Germany is totally different because GPs are not allowed to prescribe CT or MRI exams, whereas in Belgium, physicians and GPs have the freedom to do so, Ranschaert said. “This is more valuable for them than following ‘guidelines’ based upon evidence-based medicine. That’s too restrictive for them, although they claim to perform ‘evidence-based medicine.’ Nothing is less true.”
 Prof. Erik Ranschaert, PhD.
Prof. Erik Ranschaert, PhD.
Medicine in Belgium is production-based, which means that the income of doctors and hospitals is still based upon productivity, and payments are volume-based. “The more they do, the more they earn. Hospitals depend on radiology, that’s the most profitable department in most hospitals,” he continued.
The wider context
There’s a growing problem of inappropriate imaging in Europe, where up to 40% of CT exams are unnecessary, and despite rising imaging volumes, many countries lack up-to-date referral guidelines, Ranschaert noted. Belgium is facing strong pressure to reduce healthcare costs and radiation exposure.
National audits (e.g., Luxembourg, with similar Belgian-type guidelines) show that up to 39% of CT and around 21% of MRIs are deemed inappropriate -- especially those ordered by GPs, he pointed out.
In Belgium, guidelines for the prescription of CT and MRI, but these are not followed, which is a problem. For instance, one of the national guidelines for the national health insurance is that request forms need to be completed thoroughly, including symptoms, suspected diagnosis, and purpose. "From daily practice, I know that this is not followed at all," he said.
To address the issue of unnecessary exams, the ESR iGuide was introduced as a CDS system that helps physicians choose the most appropriate imaging based on patient data and evidence-based guidelines. It provides an appropriateness score, integrates with hospital IT systems, and promotes standardized, safer, and more efficient imaging workflows, he said.
“Pilot implementations across Europe show that iGuide can reduce unnecessary imaging by 7-10%, improve justification, and support compliance with EU regulations (EURATOM 2013/59). The system offers educational benefits, supports policy goals, and enhances the clinical value of imaging,” Ranschaert added.
The implementation of the PSSR and DRP may have a significant and largely positive impact on clinical practice, he said. By embedding evidence-based guidelines into the electronic ordering workflow, the system would help referrers choose the most appropriate exam upfront, and this may reduce the number of unjustified or suboptimal requests. The CDS system can streamline the imaging referral and protocoling process, especially if integrated with a hospital’s electronic health record, and it could reduce the administrative burden on radiologists and avoid delays caused by incomplete or vague clinical questions.
The ability to track trends in referral justification could help us monitor adherence to best practices, identify outliers, and support quality improvement initiatives within the department, but the actual impact will depend on how well the system is integrated with the local IT infrastructure and whether referring clinicians (especially GPs) are engaged in its use.
“In Belgium, there is no culture of following the guidelines,” Ranschaert said. “Medical doctors adhere strongly to their status of professional freedom. In my opinion, this cultural issue is a major problem.”
Also, medical doctors and GPs generally do whatever patients ask them to do because there's free competition and patients can go wherever they want. GPs are afraid of losing a patient if they don't comply with a request for a scan, he explained. The current minister of health is trying to reform the system, but this has been met by protests from doctors and dentists, who recently took part in a one-day strike.
Looking ahead
The plan to embed the CDS system into the national eHealth platform is a major step forward and technically feasible, provided close collaboration exists between hospitals, software vendors, and national health authorities, Ranshaert said. “Integration can be achieved smoothly if IT departments are involved early and standards like ICD-10 or IHE are supported. But this is a really daunting task because most IT departments already have a shortage of capacity, especially in smaller peripheral hospitals.
A critical factor is clinician adoption. “Systems like iGuide work best when referrers receive meaningful, nonintrusive feedback. If the system is too rigid or cumbersome, it risks resistance or bypass behavior. Early training and clear communication about its purpose and benefits are therefore essential,” he noted. “Without careful messaging and inclusive training strategies, there is a high risk of clinician resistance.”
The alignment with EURATOM 2013/59 and national initiatives such as BELMIP adds regulatory weight and legitimacy to the project, he noted. This will help drive adoption across hospitals, particularly if there are incentives or mandates linked to justification compliance, but convincing clinicians to participate and accept this system will be a challenge. “Efforts should not only target radiologists but also include systematic communication and incentives for referring clinicians,” he stressed.
You can read the full BELMIP EuroSafe 2025 poster on the ESR’s EPOS website. The co-authors were M. Cobbaert, G. Villeirs, M. Moreira, A. Van Schuerbeek, L. Grypdonck, K. Van Slambrouck.