The new European Society of Thoracic Imaging (ESTI) nodule management recommendations for low-dose CT lung cancer screening emphasize lesion aggressiveness, size, and morphology, while building on previous guidance.
A team led by Prof. Mathias Prokop, chair of radiology at Radboud University Center, Nijmegen, the Netherlands, and Dr. Annemiek Snoeckx, chair of radiology at Antwerp University Hospital in Belgium, published the new guidance on 1 July in European Radiology. They noted that ESTI sought a balance between mitigating the number of follow-up visits, the possibility of overtreatment, and reducing the risk of a major stage shift in developing its recommendations.
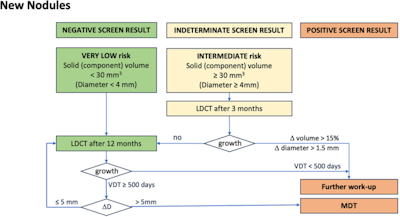 Flowchart for management of new nodules. New nodules that had been missed or not reported on previous scans are managed according to the same rules as nodules found at baseline.Courtesy Prokop, Snoeckx, ESTI; European Radiology.
Flowchart for management of new nodules. New nodules that had been missed or not reported on previous scans are managed according to the same rules as nodules found at baseline.Courtesy Prokop, Snoeckx, ESTI; European Radiology.
The guidelines emphasize categorizing by the size of the solid nodule or the solid part of a subsolid or cystic nodule. Volume is the recommended method for measurement; the authors stated that measurements taken with calipers are substantially less accurate and reproducible than volumetric measurements. However, manual diameter measurements are recommended as backup if segmentation at volumetry is found to be inaccurate and cannot be corrected. The authors gave specific guidelines for both methods of measuring, as well as for calculating the repeatability coefficient.
Additionally, volume-doubling time (VDT) is recommended here as the preferred measure for the growth rate of the tumor; the aggressiveness of the nodule is estimated from this VDT or from yearly diameter change. However, the authors cautioned that the calculation of the growth rate is affected by measurement variability, with larger error margins in cases of shorter follow-up periods and slower growth.
Furthermore, the VDT has been shown to vary among types, with solid nodules growing faster than either partially solid or nonsolid nodules. Therefore, the guidelines set the growth thresholds for stages in order that rapidly growing nodules could be identified while still small, and unnecessary follow-up could be avoided for those that are slow-growing, for which a conservative approach is generally recommended.
Likewise, as the authors stated that rapid growth is associated with aggressiveness in tumors, stage shift is also more likely in rapidly growing tumors and after longer intervals between follow-up visits, and with nodules closer in size to the next stage. Larger nodule size increases the risk for lymphatic and distant metastases, and if those metastases develop, or if a tumor stage T1a (<1 cm) at baseline develops into a tumor stage ≥T1c (≥2 cm) during follow-up, a major stage shift has occurred, according to these guidelines.
The guidelines are structured to provide management for nodules according to type, size, and morphology. They underscore again that subsolid and cystic nodules are generally less aggressive and a more conservative approach with long-term surveillance is appropriate; furthermore, new nonsolid nodules are usually infectious, and even when premalignant, are slow-growing. However, the authors also added that the development of a solid component in these nodules indicates invasiveness.
Growth with solid nodules may be variable; while rapid growth is a measure of aggressiveness, the guidelines also caution that malignant nodules may be slow-growing. For this reason, the authors added an absolute growth threshold of 5 mm: Should a slow-growing lesion increase in diameter by at least 5 mm, the decision should be made to weigh possible overtreatment against the risk from the cancer. Through this standard, the ESTI aims at "avoiding stage-shift in patients with a good life expectancy while reducing aggressive management in patients who might not profit from it."
Overtreatment is most likely to occur with slow-growing tumors, which are unlikely to metastasize, or in patients with comorbidities that are much more likely to affect their survival than the lung tumor, according to the authors.
For follow-up intervals, the ESTI team states that “[t]he nodule with the shortest follow-up interval determines participants’ management”; benign nodules should have no effect on management. Furthermore, while nodule management is based on malignancy risk, it should always take into account the lesion’s projected aggressiveness to avoid overdiagnosis and overtreatment, as well as to minimize the amount of follow-up a patient must undergo. Regular lung cancer screening should be performed at one-year intervals, the authors wrote.
Read the new ESTI recommendations here.