Its diagnostic efficacy is well established, but CT colonography (CTC) -- also known as virtual colonoscopy -- remains underutilized in many countries, according to an article posted on 31 July by Insights into Imaging.
In the article, a team led by Dr. Mehdi Cadi of the Department of Radiology, Paris Cité University, Assistance Publique Hôpitaux de Paris, and Georges Pompidou University Hospital, Paris, reflects on more than 30 years since CTC was first described. It also summarizes potential and emerging indications for the technique.
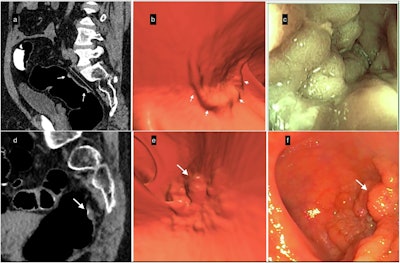 Lateral spreading tumors (LSTs). (a–c) Example of LST-non-granular (LST-NG). (a) Sagittal 2D-image with 40–400-HU abdominal window setting indicates a large 5.6-cm lesion with subtle diffuse thickening of the rectal wall (white arrows); the surface is partially covered by a thin layer of orally administered contrast agent. (b) The appearance of the villous mat on the 3D endoscopic view highlights the nodular aspect (white arrows) at the periphery of the lesion. (c) The optical colonoscopy view with the final diagnosis of a carpet villous adenoma with low-grade dysplasia. (d–f) Example of an LST-granular (LST-G) lesion. (d) Sagittal 2D image indicating nodular thickening of the rectum wall with a 10-mm nodule (white arrow). (e) The 3D endoscopic view visualized the irregular LST with a large nodule (white arrow), similar to (f) the endoscopic image obtained the same day after CTC. It confirmed the diagnosis and allowed mucosectomy with a final pathology report of a tubulous lesion with high-grade dysplasia.All images courtesy of Dr. Mehdi Cadi et al and Insights into Imaging
Lateral spreading tumors (LSTs). (a–c) Example of LST-non-granular (LST-NG). (a) Sagittal 2D-image with 40–400-HU abdominal window setting indicates a large 5.6-cm lesion with subtle diffuse thickening of the rectal wall (white arrows); the surface is partially covered by a thin layer of orally administered contrast agent. (b) The appearance of the villous mat on the 3D endoscopic view highlights the nodular aspect (white arrows) at the periphery of the lesion. (c) The optical colonoscopy view with the final diagnosis of a carpet villous adenoma with low-grade dysplasia. (d–f) Example of an LST-granular (LST-G) lesion. (d) Sagittal 2D image indicating nodular thickening of the rectum wall with a 10-mm nodule (white arrow). (e) The 3D endoscopic view visualized the irregular LST with a large nodule (white arrow), similar to (f) the endoscopic image obtained the same day after CTC. It confirmed the diagnosis and allowed mucosectomy with a final pathology report of a tubulous lesion with high-grade dysplasia.All images courtesy of Dr. Mehdi Cadi et al and Insights into Imaging
Clinical experience and research have shown that CTC is well-tolerated, minimally invasive, and comparable to optical colonoscopy in performance, the group noted. TC is highly sensitive and specific for detecting colorectal cancer, as well as polyps ≥ 10 mm years before potential malignant transformation.
It is often used as an adjunct to optical colonoscopy: after an incomplete optical colonoscopy (and may even be performed the same day) or when a patient refuses an optical colonoscopy, as well as for elderly and frail patients, for whom optical colonoscopy may not be feasible due to such issues as contraindication to anesthesia.
Furthermore, with its increased clinical use, CTC has come to be used for local colon-cancer staging, the selection of patients with severe diverticular disease for elective sigmoidectomy, and preoperative laparoscopic surgery planning. For the latter, the authors suggest that CTC offers a "one-stop shop" approach for laparoscopic surgery planning, as it enables precise localization and detailed vascular mesenteric mapping.
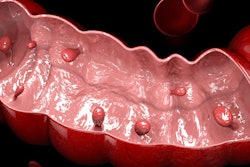
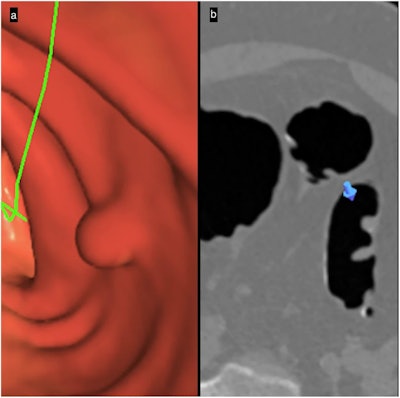 Primary 3D polyp detection: 3D-2D interaction. (a) 3D-endoscopic view makes detecting a candidate sessile polyp easier. (b) The 2D-axial image confirms the polyp’s soft-tissue value, bookmarking on the 2D image (blue arrow) the specific location shown on the 3D image.
Primary 3D polyp detection: 3D-2D interaction. (a) 3D-endoscopic view makes detecting a candidate sessile polyp easier. (b) The 2D-axial image confirms the polyp’s soft-tissue value, bookmarking on the 2D image (blue arrow) the specific location shown on the 3D image.
With the rise of neoadjuvant therapies for advanced colorectal cancer, CTC may develop a pivotal role in radiological staging, the authors write.
CTC can also be used to detect extracolonic abnormalities, highlighting its utility beyond colon cancer. Its usefulness for opportunistic screening for cardiometabolic disorders related to chronic diseases (e.g., cardiovascular diseases, sarcopenia, osteoporosis) has been evaluated, particularly in conjunction with the use of AI algorithms for the quantification of accompanying metrics such as aortic calcification, hepatic steatosis, and bone-mineral density.
CTC is a low-dose procedure, with an x-ray exposure for CTC of 1-3 mSv every three to five years, depending on the surveillance frequency, according to the authors. The low dose used has been attained through technological advances in detectors and iterative, AI-enabled reconstruction filters.
While colorectal perforation is a risk, it is very rare. Contraindications include conditions such as active inflammatory, infectious, or ischemic colitis, bowel obstruction, acute diverticulitis, and nonreducible inguinal hernia, or if the patient has undergone a polypectomy, mucosectomy, or deep biopsy recently. It is also contraindicated if the patient is pregnant or if pregnancy cannot be excluded.
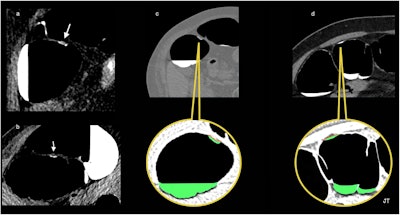 Flat-serrated lesions. This true flat polyp appears as a < 3-mm-high nonpolypoid tissue lesion spreading on the surface at a fixed location on a right lateral decubitus and (b) left decubitus positioning, and covered by a thin film of oral contrast, demonstrating the floating oral contrast-coating sign. (c) The surface of the oral-contrast sign in contact with the polyp is depicted as an undulating red line. The green is an artifice to color liquid in the colon to improve visualization. (d) The stool adhering to the colon wall in another patient appears as the contrast-agent sign in contact with the wall and is seen as a smooth and regular surface with a concave appearance (red line).
Flat-serrated lesions. This true flat polyp appears as a < 3-mm-high nonpolypoid tissue lesion spreading on the surface at a fixed location on a right lateral decubitus and (b) left decubitus positioning, and covered by a thin film of oral contrast, demonstrating the floating oral contrast-coating sign. (c) The surface of the oral-contrast sign in contact with the polyp is depicted as an undulating red line. The green is an artifice to color liquid in the colon to improve visualization. (d) The stool adhering to the colon wall in another patient appears as the contrast-agent sign in contact with the wall and is seen as a smooth and regular surface with a concave appearance (red line).
"CTC is a minimally invasive and safe examination for patients when its contraindications are respected," Cadi et al wrote.
The authors also caution that CTC’s equivalent performance with optical colonoscopy only holds true when the radiologists performing CTC are trained adequately in the procedure. They note that training for CTC is offered by professional societies throughout the world. Furthermore, they add that some societies have specific targets for training: The American College of Radiology (ACR) recommends that CTC specialists complete 50 endoscopy-verified cases every two years as continuing education, for example.
CTC offers a complementary approach when used with optical colonoscopy, can be used in situations where optical colonoscopy cannot, and its potential applications continue to broaden with increased clinical use and research.
Read the article here.