CHICAGO - Advances in procedures such as knee replacement, ligamentous reconstruction, and articular cartilage and meniscus repair have led to rapid growth in open and arthroscopic knee surgery. This has heightened demand for postoperative MRI, yet the topic is barely covered in the literature, according to Swiss researchers.
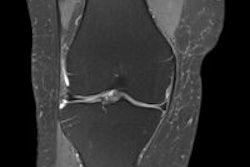
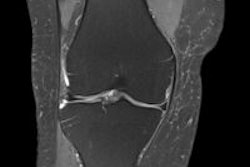
The anterior cruciate ligament (ACL) is one of the most frequently injured ligaments of the knee. During the first month after surgery, MR signal intensity of ACL grafts is usually low on T1- and T2-weighted MRI, and thus is similar to normal patellar tendon, reflecting the relatively avascular nature of the grafts, noted lead author Dr. Ralph Gnannt, from the department of radiology at Zurich University Hospital, in a comprehensive education exhibit presented at the RSNA 2011 congress.
Over time, ACL grafts will undergo a phase of remodeling during which they get enveloped by synovial tissue with graft vascularization. This results in mild increased signal intensity on T1- and T2-weighted MRI during the next 12 to 18 months, after which the signal intensity characteristics approach those of native ACL.
"Graft position and location of the femoral and tibial tunnels of the reconstructed ACL are important factors for long-term outcome," Gnannt pointed out. "Expected location of the tunnels can be evaluated on MRI using the Blumensaat line. On sagittal MRI, the anterior border of tibial tunnel opening should be located posterior to the point where the Blumensaat line intersects the tibia. At the same time, it should not be posterior to the midpoint of the proximal tibia."
If the tibial tunnel is located too far anteriorly, patients typically cannot fully extend the knee due to roof impingement. If tibial tunnels are positioned too far posteriorly or too vertically, persistent knee instability related to graft laxity is likely, he stated. The femoral tunnel should be located posterior to the intersection of the Blumensaat line and a line parallel to the posterior femoral cortex. The optimal angle of the ACL graft on coronal MRI should be less than 75° in relation to the horizontal.
Aside from surgical errors, the most common cause for failed ACL reconstruction is reinjury. Graft fixation problems may also result in ACL reconstruction failure. Biodegradable and metal interference screws, cross pins, and Endobutton cortical fixation are often used, and they may create extensive susceptibility artifacts, especially in 3-tesla MR systems.
"Posterior cruciate ligament (PCL) injury is less frequent than ACL injury," Gnannt noted. "Femoral or tibial tunnel malpositioning is also an issue in PCL reconstruction and should always be evaluated by readers. The criteria are less well-defined in the literature, which shows no consensus among orthopedic surgeons with regard to the optimal tunnel positions. Thus, radiologists should know about PCL reconstruction techniques and expected tunnel position criteria of their surgeons. The femoral tunnel is expected within the anterior 25% of the Blumensaat line."
The medial collateral ligament (MCL) has superficial and deep components and is the most frequently injured ligament in the knee. The mainstay of treatment is nonoperative, but operative management of symptomatic higher-grade injuries should be considered when laxity and instability persist, especially in high-performance athletes. Occasionally the MCL may be reconstructed in patients with complex ligamentous injury of the knee.
Acute injuries to the posterolateral corner (PLC) of the knee are often due to a multiligamentous traumatic knee dislocation, or they may be associated with acute ACL and PCL injuries, according to Gnannt. ACL reconstruction may be delayed to allow time for the PLC injury to heal or for surgical repair of the PLC, which should be performed first to prevent future ACL graft failure.
"MRI is usually performed in patients with residual or recurrent laxity as well as persistent pain after surgery," he noted. "Literature on MRI of PLC reconstruction is, however, scant. Normal postoperative graft appearance includes increased signal intensity on T2-weighted MRI as well as thickening of the graft on T1-weighted images. The site of graft disruption might be located near the femoral or tibial fixation site, which might not be visible due to metal-induced susceptibility artifacts."
Evaluation of postrepair menisci represents another challenge for radiologists because of irregular margins of the meniscus as well as linear signal granulation tissue or mature fibrocartilaginous scar tissue at the repair site. This finding persists in about half of menisci following surgical repair, at a mean follow-up of 12.9 years, he emphasized. Fluidlike signal abnormality on T2-weighted MRI is a clear indication of retears at the repaired meniscus site. A tear at a location other than the prior repair site or a displaced meniscal fragment clearly indicates new tears.
Controversy surrounds the best MR technique for imaging the postoperative meniscus, and experts disagree over whether direct or indirect MR arthrography may perform better than standard MRI in depicting retears after meniscal repair. At the Zurich center, standard MRI is used for all postoperative knees, and contrast agents are reserved for unclear cases only.
Articular cartilage surgery
MRI is the modality of choice for evaluating marrow-stimulation techniques, osteochondral grafting, and chondrocyte implantation procedures, according to Gnannt. Postoperatively, the marrow commonly shows increased signal intensity on T2-weighted MRI. In osteochondral grafting, the aim is for a congruent bone-bone and cartilage-cartilage interface, and the normal MR appearance should be that of a smooth congruent articular surface. The transplanted cartilage should demonstrate the same signal intensity as normal articular cartilage, but the gap-filling components may show persistent heterogeneous signal intensity.
"Postoperatively, there is increased signal intensity on T2-weighted MRI at donor and recipient sites, representing the healing process with fibrovascular tissue," according to Gnannt. "Usually this increased signal intensity disappears after 12 months but can be seen occasionally up to two years. Three stages of healing occur following autologous chondrocyte implantation: the proliferative phase (first six weeks), the transition phase (seven to 12 weeks), and the remodeling and maturation phase (nine to 18 months)."
During maturation, the transplanted tissue appears heterogeneous, and at full maturation it should have the same signal intensity as the adjacent articular cartilage on all standard MR sequences. Typical MRI findings in complicated or unsuccessful cases include underfilling, hypertrophy and/or fibrous overgrowth of the periosteal patch over the adjacent normal cartilage, failure of incorporation of the graft or dissociation from shearing forces with a thin fluidlike hyperintensity along the subchondral lamina or at the border zones, and increasing marrow edema and/or cyst formation subjacent to the cartilage surface.
The knee is the second most replaced joint after the hip, and MRI is often performed after total knee arthroplasty to identify problems related to infection and occult fracture (e.g., fatigue fracture of the patella), and to assess the patellar tendon, quadriceps tendon, Hoffa's fat pad, ligaments, and neurovascular injuries.
"In our experience, susceptibility artifacts induced by the prosthesis are not a significant diagnostic problem, especially when metallic artifact reduction techniques are used," concluded Gnannt. "Prosthetic shedding of metal or polyethylene is a significant late complication as it leads to hypertrophic synovium, histocytic response, and as a final result to osteolysis. On MRI, wear debris may have a tumorlike appearance, but should not be confused with malignancy."