Patients with non-small cell lung cancer (NSCLC) who smoke during the weeks they receive radiation therapy may reduce their overall benefit of treatment. Smoking has a significant negative effect as measured by several factors for assessing radiation therapy's effectiveness, according to a new study.
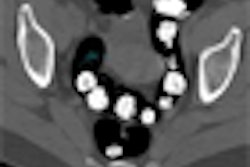
The retrospective study was published in the July 15 issue of the International Journal of Radiation Oncology, Biology, Physics (Vol. 71:4, pp. 1134-1142) and analyzed 181 patients who received radiation therapy for nonmetastatic NSCLC at the University Hospital Schleswig-Holstein in Lübeck, Germany, between January 2000 and December 2005. The research team's goal was to measure the impact on radiation therapy of three factors that can reduce tumor oxygenation: smoking during radiotherapy, respiratory insufficiency before radiation therapy, and hemoglobin levels during radiation therapy.
Tumor oxygenation is critical for achieving maximum efficacy from radiation therapy, because tumor hypoxia can produce increased resistance to tumor cell kill from radiation therapy due to the lower production of cytotoxic free radicals, resulting in less DNA damage, according to lead author Dr. Dirk Rades, a radiation oncologist at University Hospital.
The researchers suggested that smoking during radiation therapy may increase the level of carboxyhemoglobin in the blood, resulting in poorer tumor oxygenation. Prior studies have proved that smoking increases carboxyhemoglobin levels, they stated.
Results from prior studies indicate that tumor oxygenation can be affected by adequacy of the blood supply, microcirculation, and the oxygen-carrying capacity of the blood, which is represented to a certain extent by total hemoglobin level. Other important parameters may exist for tumor oxygenation in addition to total hemoglobin level.
According to the researchers, the enhanced radiation effect on patients who did not smoke during the weeks of radiation therapy may be explained by better tumor oxygenation from the improved oxygen-carrying capacity of hemoglobin due to less carboxyhemoglobin being present.
The study examined smoking's impact on 13 factors as measures of radiation therapy, including overall survival, locoregional control, and metastasis-free survival. In the study cohort, 78% of the patients were male, 22% were female, and 47% were over the age of 65. Also, 83% were diagnosed with stage III tumors and 17% had stage I and II tumors. All of the patients were smokers at the time they were diagnosed.
Of the group, 74 patients, or 41% of the total, smoked throughout their five to seven weeks of radiation therapy. Hemoglobin levels were measured each week.
A variety of univariate and multivariate analyses were conducted to identify possible relationships with outcomes. Additional prognostic factors evaluated included age, gender, Karnofsky performance score, histologic type and grade, T stage, N stage, American Joint Committee on Cancer (AJCC) stage, chemotherapy, and pack years of smoking. Subgroup analyses were also performed for patients who had undergone surgery and for those who had not.
Smoking's impact
The researchers reported that locoregional failure occurred in 76 of the 181 patients. Of these, 42 continued to smoke during radiotherapy. Tumors recurred in their lungs or regional lymph nodes between one month and 25 months.
In the 34 patients who stopped smoking prior to radiotherapy, tumors recurred in their lungs or regional lymph nodes between one month and 56 months. Of all the nonsmoking patients whose tumors recurred, the recurrence occurred later than 30 months in only one patient.
Analysis of the results indicates that smoking during radiation therapy was significantly associated with locoregional control and must be considered an independent prognostic factor, according to the researchers. The fact that the number of pack years did not significantly affect treatment outcome supports the hypothesis that the tumor oxygen status during radiation therapy was important for the radiation effect, they stated.
Abstinence from smoking did not improve the odds of having a metastasis-free survival or overall survival, however. The median survival rate for the 181 patients was 12 months.
Other results
Respiratory insufficiency was adversely associated with overall survival on multivariate analysis and locoregional control on univariate analysis. This is the first analysis of the prognostic value of respiratory insufficiency on clinical outcome for lung cancer patients, according to the authors.
By Cynthia Keen
AuntMinnie.com staff writer
July 16, 2008
Related Reading
Combining chemo and radiation improves NSCLC outcomes for elderly, April 16, 2008
Nimotuzumab boosts effect of ionizing radiation against some NSCLCs, March 31, 2008
Stereotactic single-dose radiotherapy an option for early lung cancer, August 29, 2007
Concurrent chemoradiation offers best survival in advanced lung cancer, August 20, 2007
Chemo added to radiation improves survival in elderly lung cancer patients, August 2, 2007
Copyright © 2008 AuntMinnie.com