The European Society of Breast Imaging (EUSOBI) is calling for a risk-based approach to breast cancer screening, including supplemental screening of average- to intermediate-risk women with breast MRI or ultrasound and annual breast MRI in high-risk women as young as 25.
In new general screening recommendations published 25 April in European Radiology, a team of authors led by Magda Marcon, MD, of the University Hospital Zurich made the case that shifting screening programs away from age-based population screening to pathways based on a woman’s personal risk level could improve screening perfomance. Benefits would include improved cost-effectiveness and reduction in underdiagnosis, false positives, and overdiagnosis.
“The implementation of a risk-stratified approach instead of a 'one-size-fits-all' approach may help to improve the benefit-to-harm ratio as well as the cost-effectiveness of breast cancer screening,” the authors wrote.
The announcement follows EUSOBI’s recommendation in 2022 that women with extremely dense breasts should receive screening with breast MRI. In its previous position paper on breast cancer screening released in 2016, EUSOBI focused on three priorities:
- 1st priority: Biennial screening mammography for average-risk women ages 50-69, extending up to 73 or 75 years
- 2nd priority: Biennial screening mammography from 40-45 to 49 years
- 3rd priority: Annual screening mammography from 40-45 to 49 years
The 2016 position paper also encouraged dedicated pathways to offer breast MRI to high-risk women based on national or international guidelines.
In its new general breast cancer screening recommendations, EUSOBI now recommends the following:
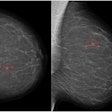
- Regular mammography should be considered the mainstay of breast cancer screening (evidence level I); digital breast tomosynthesis can be performed as an alternative. The frequency and age of stopping screening should be based on national recommendations.
- Whenever possible, risk assessment should be performed at a young age (≈25 years) to effectively tailor screening recommendations.
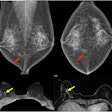
- Women at high risk of breast cancer: screening should start as early as 25 years of age with annual breast MRI (evidence level I), supplemented with mammography from age 35 to 40.
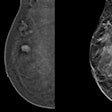
- Women at intermediate risk of breast cancer (ACR BI-RADS Atlas breast density category C and D): Supplemental screening, including digital breast tomosynthesis, breast ultrasound, breast MRI, and possibly contrast-enhanced mammography may be beneficial. The most appropriate imaging modalities should be adjusted to patient characteristics.
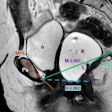
- Women with extremely dense breast tissue (breast density category D): Supplemental screening with MRI should be performed preferably every 2-3 years (evidence level I). If MRI is not available, supplemental ultrasound can be performed as an alternative although evidence is more limited.
“The current evidence supports the use of breast MRI screening in women with extremely dense breast tissue, preferably every 2-3 years (evidence level I),” they wrote. “If MRI is not available, supplemental ultrasound can be performed as an alternative, although the added value of supplemental ultrasound regarding cancer detection remains more limited.”
The authors noted that several risk prediction models can estimate an individual’s risk of developing breast cancer.
“If possible, risk assessment should be performed at a young age (approximately 25 years) to effectively tailor screening recommendations,” the authors wrote. “Individual screening recommendations should be made through a shared decision-making process between women and physicians.”
Although mammography remains a very effective imaging modality for breast cancer screening, its performance can vary depending on personal characteristics such as family history and breast density, the authors concluded. There is now evidence that considering these and some other factors to provide a more personalized screening and incorporating other screening modalities may help to further improve the early diagnosis of breast cancer, and several current studies are investigating these aspects, they stated.
Commentary from Ritse Mann
A major issue is how to create a system that is on the one hand flexible enough to allow personalization of screening and that is on the other hand simple and robust enough to offer to all women, Dr. Ritse Mann, chair of the EUSOBI scientific committee, told AuntMinnieEurope.com on 26 April.
Commenting on risk assessment at a young age (25), he said: "Only then it makes sense to search for women at substantially increased risk, and this is a first step to enable risk based screening. This recommendation also repeats clearly that we believe density on mammography should always be reported (i.e. also in screening), as it also strongly affects risk and efficacy of screening."
For high-risk women, the recommendation "propels MRI to the baseline screening modality," added Mann, a breast and interventional radiologist at the Radboud University Medical Center in Nijmegen and the Netherlands Cancer Institute in Amsterdam. "Mammography is supplemental (not the other way round), and may be helpful from 35-40, but the basis is MRI. That is in fact also new."
Overall, the authors' aim was to provide a global overview of best practice in the field of screening, he continued. "We acknowledge new technologies and have also provided some handholds on what is needed to bring new techniques to the screening realm (and what is not realistic and might even be considered unethical)."
Mann thinks the acknowledgement of underdiagnosis as a major downside of screening is also important. "False positives and overdiagnosis are commonly discussed, but the fact that we miss a lot of significant cancers in screening (particularly with mammography) is often disregarded."
Finally, the suggestion that "screening programs should be adapted to local realities -- pushing education, awareness creation and even clinical examination in low resource settings -- is important. We don’t want to push for impossible to reach goals, rather make sure that women are best served to what can be achieved locally. Many of these things may seem to be open doors, but I guess sometimes it is important to just put them on paper," he concluded.
The full European Radiology article can be accessed here.