Ultrasound is an effective modality for detecting radiolucent foreign bodies that may not be identified with radiography, but it is not always used when it should be, U.K. musculoskeletal (MSK) researchers have found.
In a study published as a EuroSafe 2025 poster, senior author Dr. Suchi Gaba, a consultant MSK radiologist at University Hospitals of North Midlands NHS Trust, and her colleague Dr. Charles Paradise noted that radiography is often being used inappropriately for foreign bodies that were expected to be radiolucent. Insufficient clinical information being submitted at the time of the imaging request contributed to the use of an inappropriate, less-effective imaging modality, they stated.
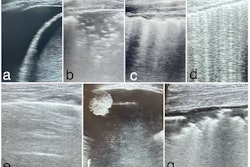
 Left: Lateral radiograph of patient with a known dermal contraceptive implant. Right: Ultrasound image in the same patient.All figures courtesy of C. Paradise and S. Gaba and presented at EuroSafe 2025.
Left: Lateral radiograph of patient with a known dermal contraceptive implant. Right: Ultrasound image in the same patient.All figures courtesy of C. Paradise and S. Gaba and presented at EuroSafe 2025.
The researchers performed a retrospective audit from January 2020 to January 2022 at a tertiary trauma hospital, with an additional 18 months for follow-up.
They used the standards that when imaging of a foreign body was requested, the referrer should explain the expected foreign body; if the suspected foreign body is radiolucent, ultrasound should be used instead of radiography. For ultrasound, the technician should include measurements for the size of the foreign body and the depth of the foreign body from the skin surface in the report; skin markings should be placed to assist with preparation for surgical removal of the foreign body, they wrote.
 Summary of the standards of the researchers' audit and their compliance.
Summary of the standards of the researchers' audit and their compliance.
From a total of 120 patients reviewed, 64 (53%) patients had the suspected type of foreign body given on the request. A total of 25 of the foreign bodies (39%) were radiopaque, and 39 (61%) were radiolucent.
However, in cases of expectation of a radiolucent foreign body, 59% of the patients reviewed underwent an x-ray first instead of ultrasound. Moreover, 19% of the patients expected to have a radiopaque foreign body underwent an ultrasound without an initial x-ray.
Of the 120 scans reviewed, ultrasound identified a foreign body in 51. Of these 51 ultrasounds, 50 included size measurements of the foreign body, 31 included the depth from the skin surface, and 12 had formal skin markings made at the time of the ultrasound in preparation for surgical removal at the referrer’s request. Of the foreign bodies seen on radiography, 73% were also seen on ultrasound.
For follow-up, the mean time interval from the initial performed radiograph to subsequent ultrasound was 46 days. Follow-up imaging was performed for 21 of the 120 patients, of whom 12 (57%) underwent radiography, one (5%) underwent ultrasound, four (19%) underwent CT, and 6 (29%) underwent MRI.
"This audit demonstrates inappropriate use of radiographs for expected radiolucent foreign bodies and sub-optimal clinical information regarding type of foreign body at the time of request -- an essential requirement to better help signpost to the most appropriate imaging modality and champion radiation protection," Paradise and Gaba concluded.
Background and context
Foreign bodies may remain undetected, even with appropriate wound examination, the authors explained. This may occur due to complex anatomical boundaries and structures, depth of the foreign body’s location, and the surrounding structures. While radiographs can identify foreign bodies made of radiopaque material such as metal and glass, radiolucent foreign bodies such as those made of vegetative matter -- e.g., wood fragments and thorns -- are not identified on radiographs, they added.
A study cited by Paradise and Gaba (Anderson et al, American Journal of Surgery, 1982: 144(1); 63–67) found that foreign bodies were missed in 38% of studied cases involving hands, which the authors noted was most likely due to the complexity of the anatomical structures involved.
However, another study by Hiremath et al (JCDR 2017: 11(7); TC14–TC16) had found that ultrasound could identify foreign bodies made of vegetative material better than either radiographs or CT. Moreover, ultrasound has been shown to effectively facilitate removal of foreign bodies, decreasing risk of tissue damage and improving outcomes, the authors noted.
Read the full EuroSafe 2025 poster here.