Researchers have described the imaging findings of Cryptococcus infection. Endemic to Australia and Papua New Guinea, it infects patients with symptoms mimicking other pathologies. While it has primarily affected the immunocompromised, it is increasingly appearing in immunocompetent patients.
Dr. India Plath, from the Department of General Surgery, Ipswich Hospital, Queensland, Australia and colleagues from the Department of Medical Imaging at Royal Brisbane and Women's Hospital in Brisbane have presented new results from eight patients who had presented with brain and pulmonary pathology and were subsequently diagnosed with Cryptococcus infection.
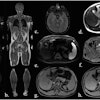
 58-year-old woman. (A) CXR frontal: right upper lobe focus of consolidation. (B) MR Brain axial T2: round lesion of right parietal lobe that is hyperintense. Left frontal lobe lesion that is also hyperintense. (C) MR Brain axial T1 + contrast: right parietal lobe lesion demonstrating peripheral enhancement. (D) MR Brain axial FLAIR: round lesion of the right thalamus, which is hypointense.All images courtesy of Dr. India Plath et al and Department of Medical Imaging, Royal Brisbane and Women’s Hospital, Brisbane; presented at RANZCR 2025 ASM.
58-year-old woman. (A) CXR frontal: right upper lobe focus of consolidation. (B) MR Brain axial T2: round lesion of right parietal lobe that is hyperintense. Left frontal lobe lesion that is also hyperintense. (C) MR Brain axial T1 + contrast: right parietal lobe lesion demonstrating peripheral enhancement. (D) MR Brain axial FLAIR: round lesion of the right thalamus, which is hypointense.All images courtesy of Dr. India Plath et al and Department of Medical Imaging, Royal Brisbane and Women’s Hospital, Brisbane; presented at RANZCR 2025 ASM.
The patients had varying symptoms, with different suspected causes, they noted in a poster presented at the annual scientific meeting (ASM) of the Royal Australian and New Zealand College of Radiologists (RANZCR), held on 23-25 October in Melbourne.
Cryptococcus infection, or cryptococcosis, is a potentially fatal fungal disease caused by inhaling Cryptococcus gattii or Cryptococcus neoformans fungus, which is found in environments like soil and bird droppings.
This variation is not at all uncommon for Cryptococcus, the authors write: “Due to the diverse range of presenting symptoms, isolated imaging findings can be mistaken for other conditions such as lung cancer with brain metastasis.” The danger in this is that prompt treatment of cryptococcal infection is critical.
The authors underscore that while imaging may point to early indications of infection, definitive diagnosis requires isolation of Cryptococcus from cerebrospinal fluid, serum, sputum, or urine. Treatment may involve months of therapy, requiring induction therapy with amphotericin B plus flucytosine, followed by consolidation and maintenance therapy with fluconazole.
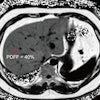
 41-year-old man. (A.) CT Chest axial: peribronchovascular lesions within the superior segment of the left upper lobe. (B.) MR C Spine sagittal T1 contrast fat sat: round lesion at the level of C3 with peripheral hyperintensity. (C.) MR C Spine sagittal T2: thick-walled lesion at the level of C3 within the cervical spine with central hyperintensity. (D.) MR Brain axial T2: small lesion of the left frontal lobe that is hyperintense with leptomeningeal enhancement. There is also associated mild cortical edema.
41-year-old man. (A.) CT Chest axial: peribronchovascular lesions within the superior segment of the left upper lobe. (B.) MR C Spine sagittal T1 contrast fat sat: round lesion at the level of C3 with peripheral hyperintensity. (C.) MR C Spine sagittal T2: thick-walled lesion at the level of C3 within the cervical spine with central hyperintensity. (D.) MR Brain axial T2: small lesion of the left frontal lobe that is hyperintense with leptomeningeal enhancement. There is also associated mild cortical edema.
Cryptococcal infection typically presents as a pulmonary infection, with a strong propensity to spread to the central nervous system (CNS). Plath et al caution that up to 40% of patients with cryptococcal CNS infections have normal CT scan results; MRI is preferred for diagnosis.
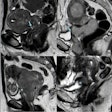
Where pulmonary imaging findings may include nodules or masses (with or without well-defined margins), pleural effusions, and lymphadenopathy, CNS findings will typically take three dominant forms, Plath et al write: meningitis, Cryptococcomas, and gelatinous pseudocysts, which the authors describe as appearing like “soap bubbles” on imaging.
The cases given include five men and three women, ranging in age from 24 to 63; some are immunocompromised (e.g., a 26-year-old woman with cystic fibrosis and a previous lung transplant). The presenting symptoms ranged widely and included both pulmonary and CNS issues, from persistent headaches, vertigo, and nausea, to paresthesia, photophobia, confusion, cough, and respiratory failure. Several of the patients were suspected of having metastatic disease. One was suspected of pneumonia; another, of an infectious process, with a possibility of malignancy. All were diagnosed with Cryptococcus infection.
The outcomes given for the patients varied, with most treated successfully when treatment was described; the immunocompromised 26-year-old woman did not survive, highlighting the dangers of the infection to vulnerable patients.
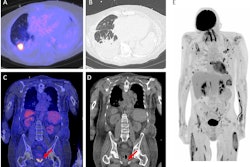
 26-year-old woman. (A.) CXR frontal: bilateral, patchy consolidation consistent with pneumonia. (B.) MR brain axial T2: extensive, small hyperintense lesions involving the basal ganglia. This is consistent with engorged and dilated perivascular spaces, which is consistent with pseudocyst formation. (C.) MR brain axial FLAIR: extensive, small hyperintense lesions involving the basal ganglia. (D.) MR brain axial T1 + contrast: there is no contrast enhancement of the lesions demonstrated on T2 and FLAIR imaging.
26-year-old woman. (A.) CXR frontal: bilateral, patchy consolidation consistent with pneumonia. (B.) MR brain axial T2: extensive, small hyperintense lesions involving the basal ganglia. This is consistent with engorged and dilated perivascular spaces, which is consistent with pseudocyst formation. (C.) MR brain axial FLAIR: extensive, small hyperintense lesions involving the basal ganglia. (D.) MR brain axial T1 + contrast: there is no contrast enhancement of the lesions demonstrated on T2 and FLAIR imaging.
Because Cryptococcus symptoms and findings can present as suggestive of other conditions, and as the fungal infection is becoming more common in Australia, the authors write that it should be considered as a possibility in cases with both lung and CNS pathology. In recognizing it as a potential diagnosis, clinicians may spare patients unnecessary diagnostic procedures and ensure prompt treatment of the infection.
The RANZCR ASM e-poster is available on the EPOS site.