Photon-counting CT (PCCT) can minimize many of the limitations of conventional CT systems by improving diagnostic accuracy and lesion characterization while reducing use of contrast agents and radiation dose in oncology imaging, according to Italian experts.
It offers energy efficiency, reduced electronic noise, intrinsic spectral capabilities, and improved spatial resolution without compromises in temporal resolution. These advantages make it especially valuable for personalized treatment planning, explained Dr. Elisa Bruno, Anna Palmisano, PhD, and colleagues from the Experimental Imaging Center at San Raffaele Hospital in Milan in an Insights into Imaging article published on 21 January.
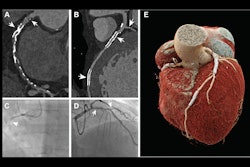
 PCCT in renal cancer. A 57-year-old woman undergoing PCCT. Axial pre-contrast (A) and venous phase (B) scans show a small exophytic nodule of the superior pole of the left kidney (11 mm), slightly hyperdense in both phases, with mild iodine uptake at the iodine map (C), suggestive of a small papillary neoplasia rather than a hemorrhagic cyst. MRI confirmed the presence of a small left kidney nodule, hypointense in the T2w image (D), characterized by mild enhancement in the arterial phase (E), with minimal washout in the venous phase (F), thus confirming PCCT suspicion. PCCT in kidney tumor surgery planning: coronal angiographic CT scan showing an exophytic heterogeneous lesion in the mid-lower right kidney (G), 5 cm in diameter, with a well-defined hypertrophic vascular pole, further highlighted on the iodine map (H). 3D reconstruction shows a double right renal artery; the lesion is supplied by the more caudal branch (white arrow in I).Bruno, Palmisano et al; Insights into Imaging
PCCT in renal cancer. A 57-year-old woman undergoing PCCT. Axial pre-contrast (A) and venous phase (B) scans show a small exophytic nodule of the superior pole of the left kidney (11 mm), slightly hyperdense in both phases, with mild iodine uptake at the iodine map (C), suggestive of a small papillary neoplasia rather than a hemorrhagic cyst. MRI confirmed the presence of a small left kidney nodule, hypointense in the T2w image (D), characterized by mild enhancement in the arterial phase (E), with minimal washout in the venous phase (F), thus confirming PCCT suspicion. PCCT in kidney tumor surgery planning: coronal angiographic CT scan showing an exophytic heterogeneous lesion in the mid-lower right kidney (G), 5 cm in diameter, with a well-defined hypertrophic vascular pole, further highlighted on the iodine map (H). 3D reconstruction shows a double right renal artery; the lesion is supplied by the more caudal branch (white arrow in I).Bruno, Palmisano et al; Insights into Imaging
“PCCT has proven capable of providing superior lesion detection, improved tissue characterization, and greater diagnostic confidence compared to conventional Energy-Integrating Detector CT across a broad spectrum of oncologic applications, from liver, pancreas, kidney, and bladder to lymph nodes, peritoneum, and bone,” they wrote.
One area where PCCT offers advantages is local staging; conventional CT, with its lower soft-tissue contrast resolution, is limited primarily to distant metastases. This feature is especially useful in certain tumors such as colorectal cancers, the authors noted.
 Patient with bilateral hip prosthesis undergoing PCCT scan. Axial and coronal views (A, C) show severe metal artifacts. Axial and coronal reconstructions after energy filtering (B, D) demonstrate a significant reduction in metal artifacts.Bruno, Palmisano et al; Insights into Imaging
Patient with bilateral hip prosthesis undergoing PCCT scan. Axial and coronal views (A, C) show severe metal artifacts. Axial and coronal reconstructions after energy filtering (B, D) demonstrate a significant reduction in metal artifacts.Bruno, Palmisano et al; Insights into Imaging
Additionally, while MRI offers better soft-tissue visualization than PCCT, it is not always practical -- access to MRI may be limited, it is expensive and time-consuming, and it may be unsuitable for claustrophobic patients or those with implanted devices. Furthermore, image quality of the two modalities may not be disparate: The authors cited a recent study on 13 patients with biopsy-proven breast cancer, in which PCCT identified a suspicious mass or nonmass enhancement in 11 of 13 cases detected by MRI, as well as three of three cases of multifocal or multicentric disease.
PCCT has also shown itself to be competitive in quality with MRI in staging breast cancer, the authors continued. “PCCT, as recently demonstrated in a small cohort of nine patients, seems to be accurate in staging and restaging of cancer compared to MRI, with an excellent correlation for tumor size before therapy (monoenergetic reconstruction r = 0.94, p < 0.001), and the iodine map (r = 0.919, p < 0.001), and good after therapy in comparison to histology (ρ = 0.786, p = 0.012).”
 PCCT in breast cancer. Chest PCCT of a 55-year-old woman suffering from dyspnea: A angiographic chest examination showing an incidental finding of a mammary nodule in the lower inner quadrant of the right breast, with a diameter of 8 mm, with rim enhancement at arterial-phase iodine map (B). For the suspicious enhancement pattern, breast ultrasound and mammography were suggested. On the same side, breast mammography shows a small speculated margin opacity containing rare microcalcifications (D), and ultrasound (C) found a solid, hypoechoic nodule with ill-defined margins, suspected for neoplasia. Ultrasound-guided core needle biopsy was performed. At histological examination, it resulted in an invasive breast carcinoma of no special type.Bruno, Palmisano et al; Insights into Imaging
PCCT in breast cancer. Chest PCCT of a 55-year-old woman suffering from dyspnea: A angiographic chest examination showing an incidental finding of a mammary nodule in the lower inner quadrant of the right breast, with a diameter of 8 mm, with rim enhancement at arterial-phase iodine map (B). For the suspicious enhancement pattern, breast ultrasound and mammography were suggested. On the same side, breast mammography shows a small speculated margin opacity containing rare microcalcifications (D), and ultrasound (C) found a solid, hypoechoic nodule with ill-defined margins, suspected for neoplasia. Ultrasound-guided core needle biopsy was performed. At histological examination, it resulted in an invasive breast carcinoma of no special type.Bruno, Palmisano et al; Insights into Imaging
PCCT has shown promise for metastases as well in different tumors, according to the Italian team. With bone metastases common (and associated with increased mortality), PCCT may be useful for identifying extremely small lesions that conventional CT may miss. Further, “the spectral capabilities of PCCT may aid in differentiating tumor progression from therapy-related changes,” the authors added.
The improved image resolution of PCCT also shows its utility in imaging lungs at a similar or lower radiation dose than conventional CT imaging, Bruno and Palmisano’s team found. A recent meta-analysis demonstrated its superior detection accuracy with lung nodules, largely due to higher image quality -- the findings showed that PCCT produced higher image quality for 30.5% to 54% of the lung nodules. The superior resolution results in better imaging of anatomical components of the lungs, as well as features of lung disease (e.g., emphysema, and alterations such as reticulation, ground-glass opacity, or mosaic patterning).
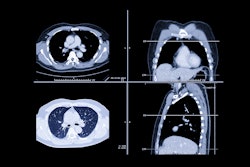
 PCCT in the assessment of lung nodules. In a 62-year-old woman, chest PCCT (A) shows a lung parenchymal irregular nodule connected to the parietal pleura of the upper right lobe, without contrast uptake on the iodine map (B), resulting suggestive of a benign nodule. FDG-PET exam confirmed the benign nature for absent FDG uptake (C). In a 62-year-old man, PCCT shows the presence of an area of structural alteration of the lung parenchyma in the context of the right upper lung lobe, in the subpleural location, characterized by ground-glass pattern with overall size of 21 × 10 mm (D), containing a completely solid nodular component approximately of 1 cm in diameter, with contrast uptake on the venous iodine map, suggestive for cancer (E). FDG-PET confirmed the presence of an FDG avid nodule (F). At histological examination, it was diagnosed as lung lepidic adenocarcinoma (pT1a pN0)Bruno, Palmisano et al; Insights into Imaging
PCCT in the assessment of lung nodules. In a 62-year-old woman, chest PCCT (A) shows a lung parenchymal irregular nodule connected to the parietal pleura of the upper right lobe, without contrast uptake on the iodine map (B), resulting suggestive of a benign nodule. FDG-PET exam confirmed the benign nature for absent FDG uptake (C). In a 62-year-old man, PCCT shows the presence of an area of structural alteration of the lung parenchyma in the context of the right upper lung lobe, in the subpleural location, characterized by ground-glass pattern with overall size of 21 × 10 mm (D), containing a completely solid nodular component approximately of 1 cm in diameter, with contrast uptake on the venous iodine map, suggestive for cancer (E). FDG-PET confirmed the presence of an FDG avid nodule (F). At histological examination, it was diagnosed as lung lepidic adenocarcinoma (pT1a pN0)Bruno, Palmisano et al; Insights into Imaging
However, despite the evident value of PCCT in oncologic imaging, the authors noted the limited availability of information on it, as well as obstacles to its broader adoption. At present, most studies on it have been small-scale investigations of its potential for early diagnosis in small cohorts; the potential for larger sets of data has not been attained yet.
PCCT also produces large volumes of high-resolution and spectral data, which can present infrastructure and financial challenges for many institutions in adopting this technology, the authors said. While the features and advantages they have described in their analysis show the potential of PCCT, “caution is needed in the interpretation of its true clinical benefits in the absence of large clinical validation.”
Read the full Insights into Imaging article here.