An award-winning Spanish survey has identified the ten pediatric neuroradiology emergencies considered to be the most challenging by radiology trainees. Failure to detect early cerebral edema is feared by 90% of trainees, while failing to spot dural sinus thrombosis in noncontrast head CT is feared by 73% of trainees.
Dr. Agustin M. Cardenas and colleagues from Hospital 12 de Octubre in Madrid conducted a survey of 30 chief or senior residents from 22 different radiology residency programs in Europe and the U.S. Of the sample, 23% were year three trainees (R3) and 77% were year four trainees (R4), and nearly a third had a program size of five or more residents a year.
The researchers, who presented their results at RSNA 2023, asked participants to select the cases that they fear the most when on call. They also asked respondents to suggest potential reasons for these weaknesses/lack of knowledge and to provide practical and feasible ways to improve the overall training in pediatric neuroradiology emergencies.
 Hospital emergency department at Aix-en-Provence, France. Courtesy of BSIP SA/Alamy.
Hospital emergency department at Aix-en-Provence, France. Courtesy of BSIP SA/Alamy.
The top 10 most challenging on-call pediatric neuroradiology cases are as follows:
- Detection of early cerebral edema. This is feared by 90% of radiology trainees because initial findings may be subtle, and there is a fear of false-positive errors and a nonfamiliarity with normal appearance of cerebral spinal fluid spaces in children, the authors noted.
- Detection of dural sinus thrombosis in noncontrast head CT: Feared by 73% of trainees because the condition is relatively uncommon and difficult to suspect clinically.
- Retropharyngeal edema versus early abscess: Feared by 63% of trainees.
- Detection of early shunt failure: Feared by 57% of trainees.
- Craniocervical junction (C1/C2) fracture versus normal developing ossification center: Feared by 57% of trainees.
- Calvarial fracture versus suture: Feared by 43% of trainees.
- Branchial cleft cyst versus retropharyngeal abscess: Feared by 37% of trainees.
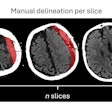
- Time estimation of heterogeneous subdural hematoma: Feared by 33% of trainees.
- Porencephalic cyst versus ventriculomegaly: Feared by 30% of trainees.
- Detection of early orbital cellulitis: Feared by 3% of trainees.
In suspected cases of early cerebral edema, it's vital to know where to look, and basal cisterns "are your friend," according to Cardenas. Get to know the normal appearance of basal cisterns, learn from normal cases, and build/develop "your internal normal template."
"As my mentor used to say, small changes in small structures can indicate big problems," he stated. "When wrong, it is better to err on the side of caution – be sensitive! Carefully, proactively review the clinical history. Altered mental status is not enough."
In any child with unexplained altered mental status and/or rapid neurologic decline, actively look for early signs of cerebral edema. "Scrutinize the subarachnoid spaces and brain sulci, particularly the vertex, as well as the basal cisterns. These early clues develop before the blurring of the gray-white matter interfaces and the impending transtentorial herniation."
More practical tips
Actively look for dural sinus thrombosis, Cardenas and colleagues recommend. "Have limited trust in your eye: do quantitative analysis of Hounsfield Units (HU) using a region-of-interest over the dural sinuses. Adjust for hematocrit. Have a low threshold to do a CT venogram, and look for delta sign. A cutoff of 58 HU and hematocrit ratios of 1.4 can lead to sensitivities of up to 100% for the diagnosis of dural sinus thrombosis."
Additionally, accurate distinction between retropharyngeal edema and early abscess has therapeutic implications, such as clinical decision-making for potential drainage, they pointed out. "It is also important to keep in mind that phlegmonous changes generally preclude fluid degeneration and capsule formation and, therefore, conspicuity of rim enhancement."
In possible cases of early shunt failure, radiologists must remember early shunt dysfunction often leads to significant changes in ventricular size but over time, cerebral parenchymal compliance may decrease.
"In older patients, small changes in ventricular size may actually reflect a significant underlying increase in intracranial pressure," the authors wrote, adding that patients with development delay may present with new vague symptoms and challenging/complex history and physical exam.
It's essential to compare new scans with any prior imaging exams and pay attention to the coronal plane because often it will better depict sulci effacement near the vertex and is less prone to comparison errors due to differences in angulation, they noted.
Editor's note: This exhibit received a certificate of merit award from the RSNA 2023 judges. The coauthors were H. Gonzalez, A. Martinez de Aragon, C. Lechuga, Z. Chen Zhou, J. Romero, E. Salvador, A. Hilario, and A. Ramos.