Almost half of patients with vocal cord paralysis (VCP) are asymptomatic, and around a third of cases have an underlying malignancy, so it's vital for radiologists to be aware that the imaging findings often precede the clinical manifestations, award-winning Spanish researchers have reported.
It's necessary to become familiar with the anatomic laryngeal landmarks, pathways of vagus and recurrent laryngeal nerves, CT features of vocal cord paralysis, and causes of recurrent laryngeal nerve paralysis, according to Dr. Alejandra Micolich Vergara and colleagues at Hospital del Mar in Barcelona. "The challenge consists of developing a keen-sighted approach to early detection of VCP and the importance of looking below the clavicles for potential causes."
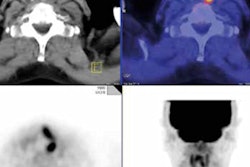
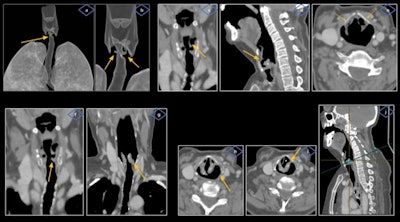
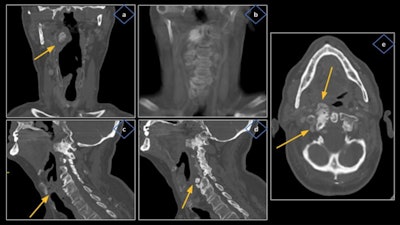 Cervical osteoarthritis caused right vocal cord paralysis (VCP) in a 69-year-old man. Thoracic images revealed severe degenerative changes of the cervical spine, especially at the level of: the soft palate, affecting the right atlantoaxial joint in the form of sclerosis, hypertrophy, and large osteophytes (a, b) projecting anteriorly with bulging of the airway (a) and occupation of the right parapharyngeal fat (e); and the cricoid ring, affecting the right uncovertebral joint of C5-C6 with an anterior osteophyte (d) that displaces the prevertebral muscles and reduces such space (c). All figures courtesy of Department of Radiology, Hospital del Mar -- Parc de Salut Mar, Barcelona, and presented at ECR 2023.
Cervical osteoarthritis caused right vocal cord paralysis (VCP) in a 69-year-old man. Thoracic images revealed severe degenerative changes of the cervical spine, especially at the level of: the soft palate, affecting the right atlantoaxial joint in the form of sclerosis, hypertrophy, and large osteophytes (a, b) projecting anteriorly with bulging of the airway (a) and occupation of the right parapharyngeal fat (e); and the cricoid ring, affecting the right uncovertebral joint of C5-C6 with an anterior osteophyte (d) that displaces the prevertebral muscles and reduces such space (c). All figures courtesy of Department of Radiology, Hospital del Mar -- Parc de Salut Mar, Barcelona, and presented at ECR 2023.VCP is the loss of mobility of the true vocal cords secondary to a mechanical cause infiltrating the glottis or a neural lesion affecting the vagus or recurrent laryngeal nerves, and these nerves provide motor innervation to the intrinsic muscles of the larynx and travel a long distance from the skull base into the upper mediastinum, they explained.
"Most cases of VCP are unilateral due to a compressive mass, although up to a third may be bilateral," the researchers continued. "VCP can be classified in central or peripheral, with central causes being about 10%, and the vast majority are peripheral."
The main symptom of unilateral VCP is dysphonia, but it can also manifest as hoarseness, aspiration episodes, liquid dysphagia, vocal fatigue, and shortness of breath, and up to 40% of patients with unilateral VCP are asymptomatic at the time of diagnosis, they noted in an e-poster that received a cum laude award at ECR 2023.
Once VCP is suspected, patients must undergo a clinical evaluation of the larynx followed by a thorough head and neck radiological evaluation.
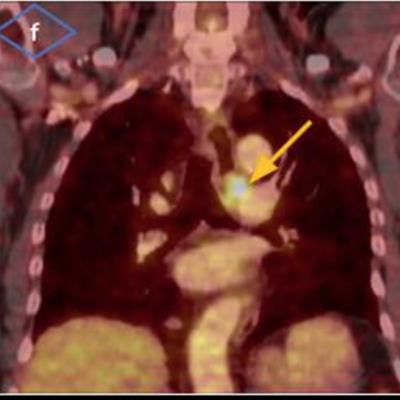
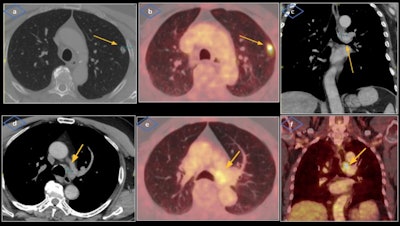 Stage III non-small cell lung cancer caused left VCP in a 71-year-old man with history of smoking and asbestos exposure, presents with five months of dysphonia with weight loss. Laryngoscopy showed signs of left VCP. Cervicothoracic contrast-enhanced CT was performed revealing a solid pulmonary nodule located in the periphery of left upper lobe (a) and a large mediastinal conglomeration of lymphadenopathies located at the left paratracheal station (d), probably injuring the course of left recurrent laryngeal nerve at the aortopulmonary window (c). PET/CT showed intense metabolic activity of the solid nodule and adenopathic conglomerate (b, e, f).
Stage III non-small cell lung cancer caused left VCP in a 71-year-old man with history of smoking and asbestos exposure, presents with five months of dysphonia with weight loss. Laryngoscopy showed signs of left VCP. Cervicothoracic contrast-enhanced CT was performed revealing a solid pulmonary nodule located in the periphery of left upper lobe (a) and a large mediastinal conglomeration of lymphadenopathies located at the left paratracheal station (d), probably injuring the course of left recurrent laryngeal nerve at the aortopulmonary window (c). PET/CT showed intense metabolic activity of the solid nodule and adenopathic conglomerate (b, e, f).The cross-sectional imaging modality of choice is contrast-enhanced CT, and PET/CT may also have a role. The CT exam must include the upper mediastinum up to the aortopulmonary window and the scan should be acquired during a period of quiet respiration, so the cords are in an abducted position, the authors added.
"The vagus and recurrent laryngeal nerves cannot be directly visualized on CT; therefore, it is imperative for radiologists to recognize their expected courses so we don't miss out on pathologies that may have more significance than the VCP itself," they pointed out.
VCP can be reliably identified on CT due to characteristic findings, although careful evaluation must be carried out by appropriately handling the scan planes of the glottis so potential pitfalls and mimics can be avoided.
 Internal bilateral laryngoceles led to left VCP in a 64-year-old woman with a history of smoking and chronic obstructive pulmonary disease. She was referred to the otorhinolaryngologist because of chronic dysphonia and dysphagia. Laryngoscopic evaluation showed left VCP. A contrast-enhanced neck CT revealed the presence of bilateral air-filled lesions (more prominent on the left side) located at the level of laryngeal ventricles (a-d), inside the paraglottic space bound by the thyroid cartilage (e). Also visible are signs of left VCP with asymmetric enlargement of both pyriform sinuses, with left side predominance (h) and anteromedial rotation of left arytenoid cartilage and vocal cord displaced medially (g, i), disclosing the "pointing" sign on coronal view (f) and the "sail sign" (*) on axial oblique plane (j).
Internal bilateral laryngoceles led to left VCP in a 64-year-old woman with a history of smoking and chronic obstructive pulmonary disease. She was referred to the otorhinolaryngologist because of chronic dysphonia and dysphagia. Laryngoscopic evaluation showed left VCP. A contrast-enhanced neck CT revealed the presence of bilateral air-filled lesions (more prominent on the left side) located at the level of laryngeal ventricles (a-d), inside the paraglottic space bound by the thyroid cartilage (e). Also visible are signs of left VCP with asymmetric enlargement of both pyriform sinuses, with left side predominance (h) and anteromedial rotation of left arytenoid cartilage and vocal cord displaced medially (g, i), disclosing the "pointing" sign on coronal view (f) and the "sail sign" (*) on axial oblique plane (j).Micolich Vergara, who is currently in her fourth year of radiology residency, told AuntMinnieEurope.com that the team in Barcelona is keen to undertake further studies in this area and collaborate with other groups.
To view the whole ECR 2023 poster and learn more about the full range of cases, go to the EPOS section of the congress organizers' website. The co-authors of the ECR e-poster were Dr. Jaume Capellades, head of neuroradiology, and Dr. Flavio Zuccarino, head of thoracic imaging, both at Hospital del Mar.