Does yearly mammographic surveillance put a large number of young breast cancer patients at further risk -- and could there be a targeted approach to the follow-up of these women? That was the idea raised in a talk at the recent UK Imaging & Oncology (UKIO) Congress.
In the U.K., around one in seven women develop breast cancer, with approximately 9% of these cancers diagnosed in young women under the age of 44, noted Heather Mower, an advanced practitioner radiographer from the Northern Devon Healthcare National Health Service (NHS Trust).
Guidelines recommend annual mammography until the screening age of 50 for those who have had treatment, which means that very young women are subject to multiple mammograms, she told attendees at the virtual UKIO meeting.
"Mammogram is the only method offered routinely to young women, despite the fact that [they] have dense breast tissue with reduced mammographic sensitivity, are more likely to be diagnosed with high-grade tumors and to have poor prognostic factors -- and the lifetime risk for developing radiation-induced cancer is highest in younger women," Mower said. "There is no known trial as yet seeking a targeted approach to surveillance for younger women who are more at risk of radiation-induced cancers."
Mower and colleagues retrospectively studied a single symptomatic breast unit, in which women were diagnosed between 1 January 2010 to 31 December 2019.
During this period 1,240 cancers were diagnosed in women, the youngest patient being 26. Of these diagnoses, 102 cancers were detected in women under the age of 44. Four of these women were diagnosed with two separate (nonmetastatic) cancers within this time period.
On average over the 10 years, 8% of women diagnosed with breast cancer were under the age of 45. The majority of these cancers were high-grade cancers, with 51% deemed grade III. While the majority had a breast density score of BI-RADS B, a large proportion had scores of C and D, denoting dense and extremely dense breast tissue.
Furthermore, 16% of the cancers were mammographically occult, and of these, the number of mammographically occult cancers was highest in the women with extremely dense breasts (44%).
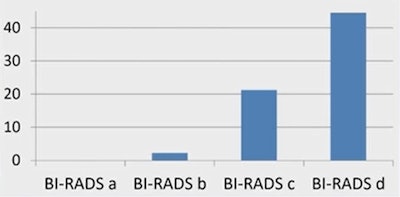 Graph showing mammographically occult cancers, the highest number occurring in dense breasts. Graph courtesy of Heather Mower and colleagues.
Graph showing mammographically occult cancers, the highest number occurring in dense breasts. Graph courtesy of Heather Mower and colleagues.Radiation dose
The average number of projected surveillance mammograms was 11 -- the highest number being 24 -- and extrapolating the mean glandular dose of 3 mGy per mammogram, these women would receive an average 33 mGy, and for the youngest 72 mGy, before entering the NHS screening program at the age of 50.
A total of 33 women stopped the surveillance prior to reaching screening age and from the remaining women, only three were offered annual MRI.
"Some women are recommended for annual mammography for up to 24 years, which puts them at increased risk of developing a radiation-induced cancer. A surveillance method with less or no radiation should be offered to all women," she said. "Further data is required to assess whether other imaging such as digital breast tomosynthesis, MRI, or ultrasound could be incorporated for the surveillance or partial surveillance of these women."
Recall scrutiny
Keeping MRI recall rates in breast cancer screening below the expected standard of 7% appears to be challenging, according to published studies, but is it impossible? Attendees at UKIO 2021 also heard how one U.K. research team put it to the test, finding that experienced MRI readers and strict protocols will help attain targets.
In the U.K., women at very high risk of breast cancer, which includes high-risk genetic mutation carriers or who have had previous radiotherapy to breast tissue, are entitled to annual MRI screening with or without mammography.
 A 32-year-old patient with the BRCA-2 gene underwent her second MRI screen. Left images show a T2 sequence showing low signal intensity fibroadenoma with corresponding high apparent diffusion coefficient, and the ultrasound correlate. On the right is the maximum-intensity projection, the subtraction images postgadolinium, and the high-resolution delayed T1 with fat-suppressed gradient echo. These show new segmental nonmass enhancement. Images courtesy of Dr. Lucinda Frank and colleagues.
A 32-year-old patient with the BRCA-2 gene underwent her second MRI screen. Left images show a T2 sequence showing low signal intensity fibroadenoma with corresponding high apparent diffusion coefficient, and the ultrasound correlate. On the right is the maximum-intensity projection, the subtraction images postgadolinium, and the high-resolution delayed T1 with fat-suppressed gradient echo. These show new segmental nonmass enhancement. Images courtesy of Dr. Lucinda Frank and colleagues.According to the NHS best practice, this group's annual MRI is double read, with at least one of the readers experienced in 100 MRI scans per year. The guidance also stipulates that the target minimum standard recall rate should be kept below 10% but the expected standard is set at under 7% per year, noted Dr. Lucinda Frank, radiology registrar at Cheltenham General Hospital, Gloucestershire NHS Foundation Trust, who presented an audit of recall rate and other key performance indicators in high-risk breast MRI screening.
"The expected recall rate of 7% has proved difficult to attain in published studies. Our aim was to evaluate the recall rate in our unit, evaluate the cancer detection rate (CDR) and assess any temporal trends," noted Frank, who pointed to recall rates of over 10% in the literature.
The team studied all high-risk screening MRI scans between January 2014 and September 2019, and it reviewed any cases with classifications of MRI 3 (indeterminate), 4 (suspicious), and 5 (malignant), to determine how the case was assessed and the outcome, whether the case was a prevalent or incident screen, and to look for trends over time. The group also searched local databases to try and identify any interval cancers.
Results showed that there were 283 screening episodes in the time period, which comprised 90 prevalent screens and 193 incident screens. A total of 19 patients were recalled for assessment. This meant that the overall recall rate was 6.7%, with a 13.3% recall rate in prevalent screens and a 3.6% recall rate in incident cases. The recall rate varied between 3% and 9% each year of the study period, and except in 2014, more prevalent screens were recalled than incident screens.
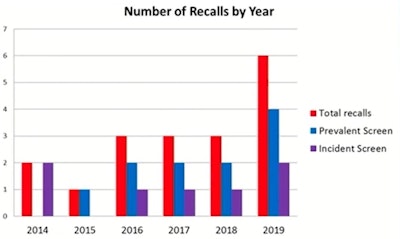 Graph courtesy of Dr. Lucinda Frank and colleagues.
Graph courtesy of Dr. Lucinda Frank and colleagues.Five cancers and no interval cancers were diagnosed during the study period. Due to the relatively small numbers included in the study, there were some years where there was no cancer detected. Overall cancer detection rate was 17.6 per 1000 and a positive predictive value (PPV) for recall of 26%, in line with the published literature, Frank told attendees.
The research team also revealed that of the recalled cases, three of 19 were deemed unnecessary: In one case there was significant movement artifact, and in another, the diffusion-weighted imaging (DWI) sequences were misinterpreted. However, these occurred before protocols changed, which led to an adjustment of T2-weighted sequence, higher-resolution DWI, and routine evaluation of postcontrast subtracted series, according to Frank.
Frank noted that the department's recall rate of 6.7% meets the expected standard of under 7%, which is better than the recall rates described in the literature. The researchers believe the unit met this target because of two key factors:
"We feel that having a small number of experienced MRI reporters and a rigorous protocol has helped achieve this standard. DWI and subtraction sequences are invaluable for problem-solving particularly in prevalent screens," Frank noted.