It's official: The COVID-19 pandemic has induced widespread insomnia, anxiety, and depression among radiologists. A large French survey has confirmed this, but it has also shown that access to logistical and psychological support has been easier in public rather than private hospitals during the pandemic.
The survey results were published online in the European Journal of Radiology on 15 September. Analysis of the answers revealed that past medical history of respiratory and psychiatric disease, exposure to COVID-19 (working in a high-density area or COVID-19-related activity), and restricted access to COVID-19-related information were shared risk factors for anxiety or depression.
Furthermore, responses pointed to the major socioeconomic impact of the crisis, especially in private practice, and working in a public hospital was a protective factor against psychological symptoms.
"Working in a public hospital may also have resulted in more frequent opportunities for radiologists to receive logistic support from their institution as well as psychological support from their colleagues and/or dedicated services," noted lead author Dr. Marie Florin, a radiologist at the Georges Pompidou European Hospital in Paris, and colleagues.
The authors noted that the apparent protective effect of working in public hospitals may be related to the more frequent feeling of usefulness for hospital radiologists. They also pointed to societal praise of care work provided by hospital workers as a possible short-term protective factor.
Florin et al added that their findings should trigger the implementation of protective measures: Radiologists working in private practice, in a high COVID-19-density area, managing patients with COVID-19, and who have past medical history of respiratory and psychiatric disease seem to be the most at risk and should be closely monitored and provided with increased access to medical education via webinar or e-learning.
On the front line
Commenting on the survey, Dr. Robert Lavayssière, staff radiologist and CEO of Centre d'Imagerie Paris-Nord, Sarcelles, acknowledged that the physical and mental strain on staff has been significant since March.
"The first wave effect is not behind us: People, including doctors and other personnel, underwent a huge shock and consequences are still undermining their lives," he told AuntMinnieEurope.com. "In the private sector, for about three months imaging exam turnover was only 15% of the usual figures, and although we got partial funding from the government, the recovery will be slow and somewhat difficult. But, we are still alive!"
Lavayssière, who is also general manager of VIDI (the national French network of 46 radiology clinics) and past vice president of the national union of private radiologists (Fédération Nationale des Médecins Radiologues, FNMR), added that there was still a huge mental dichotomy between the perception of the public and private sectors, pointing to how public compliments and praise were addressed to the public sector, without much acknowledgement of private doctors during the pandemic.
 Are medical imaging staff in private hospitals as valued and praised as colleagues in public hospitals? These radiographers work at Centre d'Imagerie Paris-Nord, Sarcelles. From left to right: Thierry, Benoît, Damien, and Hassina. Image courtesy of Dr. Robert Lavayssière.
Are medical imaging staff in private hospitals as valued and praised as colleagues in public hospitals? These radiographers work at Centre d'Imagerie Paris-Nord, Sarcelles. From left to right: Thierry, Benoît, Damien, and Hassina. Image courtesy of Dr. Robert Lavayssière.He noted that resentment increased when there was discrepancy among premiums being awarded at first to public hospital staff and thereafter to some staff in private clinics but not others, with "elusive answers" from the Ministry of Health and regional health agencies when questioned on the matter.
"It should be remembered that our staff and doctors have deeply invested their energy in fighting the virus, and the death toll among physicians and staff has been much higher in private practice -- and not just because of less protective equipment," he said.
Key findings
The anonymous survey was conducted in mid-April, during the fifth week of lockdown, by the national society of radiology (Société Française de Radiologie, SFR), the FNMR, the union of hospital radiologists (Syndicat des Radiologues Hospitaliers, SRH), the national union of radiology residents (Union Nationale des Internes de Radiologie, UNIR), and the national college of radiology teachers (Collège des Enseignants de Radiologie Français, CERF).
The five bodies emailed their members with the link to the questionnaire three times in order to increase response rate, and they provided nine days for online response. Participants answered questions about changes in their work organization and the economic impact of the pandemic, while the authors measured symptoms of insomnia, anxiety, and depression through two validated scales: the Insomnia Severity Index (ISI) and the Hospital and Anxiety Depression Scale (HADS).
A total of 1,515 radiologists (21% response rate) responded to the online questionnaire, according to the study. Of the 1,515 participants, 671 were women (44.3%), and a slight majority (n = 809, 53.4%) worked in private practice. Among all survey respondents, 674 (44.5%) worked in a region with a high rate of patients hospitalized for COVID-19, and 40 (2.6%) had tested positive for SARS-CoV-2.
A slight majority of participants (n = 809, 53.4%) reported that less than 25% of their activity was related to COVID-19, that they had to manage severe patients (n = 913, 60.3%), and that they had co-workers with COVID-19 (n = 873, 57.6%). In addition, 1141 respondents (75.3%) indicated they did not have sufficient access to protective equipment.
Overall, radiologists working in public hospitals were more likely to work in a high COVID-19 density area, to have a COVID-19 related activity, to manage patients with severe COVID-19, to have co-workers with COVID-19, to fear contaminating their relatives, and conversely, were less likely to have insufficient access to protective equipment (all p-values < 0.001).
Furthermore, 1,308 radiologists (86.3%) had to decrease their activity during lockdown. A total of 1,061 (70%) responders felt concerned about the management of non-COVID-19 patients, and 336 (22.2%) either increased their teleradiology activity or started to work via teleradiology for the first time, with 166 (11%) helping co-workers in other departments such as the emergency department.
Although 627 participants (41.4%) did not express any change in their relations with co-workers, 519 (34.3%) declared they had lost contact with co-workers. Overall, 463 (30.6 %) reported that they were negatively impacted in their medical education.
Among private practice radiologists, 675 (83.4% of 809) received financial aid from the government. Radiologists working in public hospitals decreased their activity less than those in private practice and had more working hours. They were also more likely to be reassigned to other departments, to experience a negative impact on their education, and to fear a work overload after the crisis. Conversely, public hospital radiologists were more likely to feel useful, less likely to have no more contact with their co-workers, and less likely to be concerned by a negative impact for the radiology structure they worked in (all p-values < 0.001).
Depression and anxiety
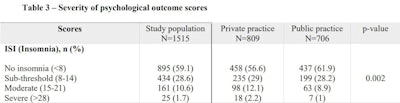
In the survey, 620 (40.9%), 513 (35%), and 464 (30.6%) participants respectively indicated symptoms of insomnia, anxiety, and depression. Respectively, 186 (12.3%), 222 (14.6%) and 188 (12.5%) participants self-reported "moderate to severe" insomnia and symptoms corresponding to definite cases of anxiety and depression. Radiologists working in private practice were significantly more likely to experience symptoms of insomnia and depression (p-values = 0.002 and < 0.001, respectively).
The authors stated that the lack of sufficient protective equipment, increase of teleradiology activity, and negative impact on education were risk factors for insomnia (odds ratio [OR] = 1.7, 1.5, and 2.5, respectively). Conversely, living with another healthcare worker and working in public hospitals were protective factors (OR = 0.6 and 0.4, respectively).
With regard to anxiety symptoms, being female, having a previous medical history of respiratory and psychiatric disease, working in a high COVID-19 density area, having a COVID-19-related professional activity, and experiencing a negative impact on education were risk factors (OR = 1.7, 2, 1.9, 1.5, 1.2, and 2.1, respectively).
Similarly, radiologists who have previous respiratory or psychiatric history, were COVID-19 positive or symptomatic, and were impacted in their education were more likely to report symptoms of depression (OR = 2.7, 2.4, 1.7, and 2.8, respectively). As for insomnia, working in a public hospital was a protective factor against anxiety and depression (OR = 0.6 and 0.5).
The study authors noted that though the sample size was large and had a wide range of variables, a limitation of the recent survey lay in the low response rate (21%) of emailed members. Furthermore, Florin and colleagues found no prepandemic data on the psychological status of radiologists and therefore couldn't determine any pandemic-related increase in anxiety and depression levels. The authors also noted that the outbreak's long-term impact on radiologists would require further investigation.