Radiology researchers from the north of Spain have received a prestigious award on the opening day of ECR 2020 Online for their presentation about five practical ways to master unusual CT findings in cancer patients.
 Dr. Ainhoa Viteri Jusué from Bilbao.
Dr. Ainhoa Viteri Jusué from Bilbao."Reading studies of cancer patients is challenging because of the complexity of the disease and the treatments. We have tried to help facing that challenge by reviewing some principles that are common to many areas of radiology, providing useful tips and warning of possible pitfalls," explained Dr. Ainhoa Viteri Jusué, a radiologist from Bilbao, and her colleagues at the University Hospital of Araba, Vitoria-Gasteiz.
The researchers emphasize the need for radiologists to think beyond tumors and metastases when interpreting oncology exams.
"Many mistakes may be prevented by internalizing these principles and using them when reading cancer studies," added the group, who received a magna cum laude award from the organizers of ECR 2020, which is taking place from 15 to 19 July.
Fear of missing tumor-related lesions
When faced with CT studies of cancer patients, radiologists fear missing tumor-related lesions. But misdiagnosis of lesions unrelated to the tumor as disease progression or recurrence can also have a negative impact on the diagnostic and therapeutic management of cancer patients.
Most findings in oncologic patients will be tumor- or treatment-related, followed closely by infections or thrombosis. Some cases don't fit in these boxes and are easy to mistake for cancer manifestations, particularly if radiologists are not aware of the less common but very characteristic findings, according to Viteri Jusué and colleagues.
For ECR 2020, the team's objective was to describe unusual CT findings in cancer patients that are not tumor-related and provide advice that can help to correctly interpret images. These were their five main tips:
1. Use optimal technique for acquiring and interpreting images
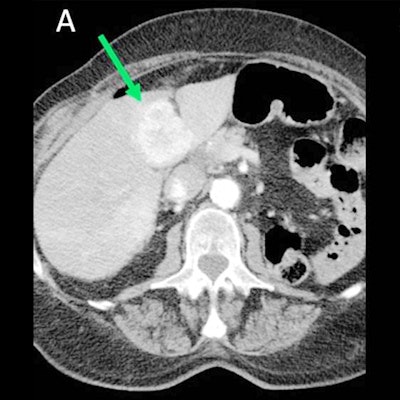
Choosing the most appropriate CT protocol is vital, they stated. For instance, hypervascular metastases are more conspicuous in the arterial phase (see figure).
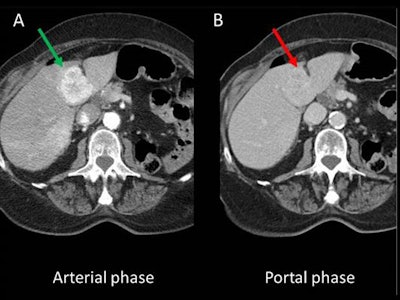 A dedicated CT protocol for typically hypervascular tumors should include the arterial phase. A: Hepatic metastasis of renal cell carcinoma hypervascular in the arterial phase. B: In the portal phase, it is almost isodense with the rest of the parenchyma and becomes much less conspicuous. All figures courtesy of Dr. Ainhoa Viteri Jusué, presented at ECR 2020.
A dedicated CT protocol for typically hypervascular tumors should include the arterial phase. A: Hepatic metastasis of renal cell carcinoma hypervascular in the arterial phase. B: In the portal phase, it is almost isodense with the rest of the parenchyma and becomes much less conspicuous. All figures courtesy of Dr. Ainhoa Viteri Jusué, presented at ECR 2020.Also, make sure you choose the right window display; review the soft tissues with a narrower window, which helps detect some lesions less conspicuous because of their density, especially in atypical locations that tend to go unnoticed, such as intramuscular metastases, bowel implants, and spinal canal lesions, they continued. If necessary, reconstruct the acquired data again. Use software that reduces metal artifacts or expand the field-of-view if any area of interest is missing -- often in the neck, shoulders, and peripheral soft tissue.
2. Remember the relevant anatomy in oncologic imaging
Radiologists should suspect that a lesion is not related to the patient's known cancer when it is in a very atypical location for that tumor, when its morphological features are clearly different from those of the primary tumor and the rest of the metastases, and when its response to treatment diverges from the rest of the lesions.
Ectopic tissue foci of different glands may simulate nodules or adenopathies, for instance. To avoid confusing these findings with tumor lesions, remember the embryogenesis of these organs. Also, these foci of ectopic tissue have a typical location, and this location's CT density and its MR signal are the same as those of the normal gland. The two most characteristic cases of ectopic tissue mimicking malignancy are hyperdense nodules of ectopic thyroid tissue in the neck or upper mediastinum along the migration route of the gland during embryonic development and foci of heterotopic pancreatic tissue in the wall of the digestive tract.
3. Keep in mind systemic manifestations of cancer and their imaging features
"Not everything is a space-occupying lesion!" the authors noted. "Although radiologists tend to think of cancer as space-occupying lesions, cancer is a heterogeneous group of diseases with systemic manifestations. Many times we can be the first to detect these systemic phenomena if we are aware of their imaging features. The two most obvious examples are the predisposition to thrombosis and infections."
4. Effects of systemic therapy can simulate tumor spread
To read cancer patients' studies, it is essential to know what treatment the patient is receiving and when to assess response and toxicity. Moreover, some side effects of therapeutic drugs can be confused with tumor progression, but they may be drug-specific and not present in the baseline study.
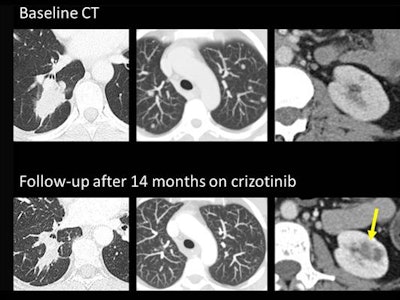 Crizotinib-induced complex renal cysts can be mistaken for malignant lesions. Top row: Baseline CT scan of a woman with stage IV ALK-mutated lung adenocarcinoma (right lower lobe mass and bilateral lung metastases) and tiny uncomplicated cortical renal cysts. Lower row: Follow-up, 14 months on crizotinib, partial response (decreased size of the right lower lobe mass and disappearance of pulmonary nodules). Development of complex cystic masses in both kidneys is consistent with crizotinib-induced renal cysts (arrow).
Crizotinib-induced complex renal cysts can be mistaken for malignant lesions. Top row: Baseline CT scan of a woman with stage IV ALK-mutated lung adenocarcinoma (right lower lobe mass and bilateral lung metastases) and tiny uncomplicated cortical renal cysts. Lower row: Follow-up, 14 months on crizotinib, partial response (decreased size of the right lower lobe mass and disappearance of pulmonary nodules). Development of complex cystic masses in both kidneys is consistent with crizotinib-induced renal cysts (arrow).To illustrate their point, the authors used the case of crizotinib-induced complex renal cysts. Crizotinib is a c-kit tyrosin-kinase inhibitor used in ALK-mutant lung adenocarcinoma. Renal cysts grow or appear "de novo" (anew) during treatment in up to 16% of patients treated with crizotinib, and around a quarter of them are complex. They should be recognized, and do not mistake them for renal metastases or renal tumors. The cysts lack clinical relevance and usually regress at the end of the treatment, the researchers pointed out.
5. Reviewing the medical record and old exams may prevent mistakes
Sequelae of remote diseases and treatments may simulate metastases, according to Viteri Jusué and her colleagues. The following four cases were initially mistaken for metastatic disease at the authors' hospital: tick-borne lymphadenopathy mimicking nodal recurrence, thoracic splenosis mimicking pleural implants, talc pleurodesis sequelae mimicking pleural implants, and dropped gallstones mimicking peritoneal implants.
A careful review of the medical record can be key to avoiding a definitive misdiagnosis, they concluded.
Editor's note: To view the authors' full e-poster, go to the European Society of Radiology's EPOS website. Also, you can listen to the Voice of EPOS oral presentation (VoE 140).