Dedicated contrast-enhanced breast CT is advancing as a tool for clinical care due to its 3D high spatial resolution, but variations persist in the acquisition protocols, particularly the timing of contrast-agent administration. Dutch researchers have tried to resolve this issue.
Τhe impact of the timing of contrast agent administration on signal intensity enhancement within lesions and areas of background parenchymal enhancement (BPE) is overlooked, according to Dr. Marialena Tsarouchi, PhD, a postdoctoral researcher in medical imaging at Radboud University Medical Center, Nijmegen, and the Netherlands Cancer Institute in Amsterdam, and colleagues.
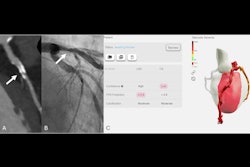
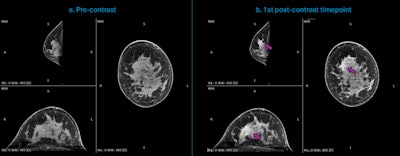 Dedicated breast CT acquisitions of a 44-year-old woman with newly diagnosed invasive ductal carcinoma (IDC) of high aggressiveness (grade 3) in the right breast. (a.) Multiplanar reconstruction of the precontrast acquisition (t = 0 seconds); (b.) Multiplanar reconstruction of the first acquired postcontrast timepoint (t = 90 seconds), indicating the enhancing malignant lesion (purple arrow), in a case with strong background parenchymal enhancement (BPE). Courtesy of Dr. Ritse Mann, NKI, Netherlands Cancer Institute.
Dedicated breast CT acquisitions of a 44-year-old woman with newly diagnosed invasive ductal carcinoma (IDC) of high aggressiveness (grade 3) in the right breast. (a.) Multiplanar reconstruction of the precontrast acquisition (t = 0 seconds); (b.) Multiplanar reconstruction of the first acquired postcontrast timepoint (t = 90 seconds), indicating the enhancing malignant lesion (purple arrow), in a case with strong background parenchymal enhancement (BPE). Courtesy of Dr. Ritse Mann, NKI, Netherlands Cancer Institute.
The researchers conducted a study to find the optimal postcontrast time point through in-vivo measurements of contrast signal intensity over time and image quality metrics. They presented their findings at the European Society of Breast Imaging (EUSOBI) annual meeting, held recently in Aberdeen, U.K.
They enrolled patients with 30 breast cancers and scanned them using the dedicated breast CT scanner with standard acquisition parameters. Each patient underwent a precontrast scan, followed by four postcontrast scans at 20-second intervals starting at 90 seconds after the end of contrast injection.
The researchers acquired, reconstructed, and registered the images. They performed temporal subtraction by subtracting the precontrast from the registered postcontrast images to highlight the lesion-related signal intensity enhancement.
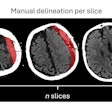
“Regions of interest were manually delineated on representative 2D coronal slices within the most enhancing part of the lesion (SLE) and the area of the surrounding fibroglandular tissue showing most BPE (SBPE),” they explained. “Registration allowed for the propagation of all the ROIs on pre-, postcontrast, and on the subtracted images.”
To evaluate the signal intensity contrast between lesions and BPE, the team calculated contrast-to-noise ratios (CNRs) for each case, time point, and subtracted images.
 Dr. Marialena Tsarouchi, PhD.
Dr. Marialena Tsarouchi, PhD.
The mean contrast-enhanced signal intensity of the lesions (μSLE = 123.8 Hounsfield units [HU]) was highest at the first postcontrast time point (90 seconds), with an average increase of 59.6 HU compared to the baseline. No relevant washout was observed over the following time points (p > 0.05), but later time points showed increased BPE, achieving the highest mean signal intensity (μSBPE = 108.3 HU) at the fourth postcontrast time point (t = 150 seconds). The average CNR across the 30 cases showed the highest values (CNR = 2.23) at the first time point (t = 90 seconds) and (CNR = 1.62) at the first subtracted image.
“Contrast enhancement and image quality metrics proved that the optimal postcontrast time point is 90 seconds,” Tsarouchi stated. “As BPE increases in later time points, scanning earlier may improve lesion detection.”
Focus on AI advances
AI, particularly deep learning-based models, shows strong potential in noninvasive axillary lymph node assessment using contrast-enhanced CT in breast cancer patients, a U.K. research team told attendees at the EUSOBI 2025 meeting.
“These models may support improved preoperative staging and reduce the need for invasive biopsies,” explained Dr. Julie Cox, a consultant radiologist at County Durham and Darlington NHS Foundation Trust. “However, widespread clinical application will require multicenter validation, standardized imaging protocols, and integration with explainable AI techniques to enhance clinical trust and decision-making.”
Along with her colleagues Dr. Amir Bhatti and Dr. Amir Atapour-Abarghouei, she conducted a systematic search in Embase, Medline, the Cochrane Library, and Google Scholar from January 2010 to September 2024. The team included studies that involved AI-based analysis of axillary lymph nodes on CT scans in breast cancer patients. Quality was assessed using the QUADAS-2 tool, and data were narratively synthesized according to PRISMA and ESRC guidelines. Five retrospective cohort studies met the inclusion criteria.
“All included studies were single-center retrospective designs from China and South Korea,” noted Cox, who was chief investigator for the Multidetector Computed Tomography Improving Surgical Outcomes in Breast Cancer (MISO BC) trial, which investigated whether CT an be used to accurately determine if breast cancer has spread from the breast to the lymph nodes in the armpit. “AI techniques included convolutional neural networks (CNNs) and traditional machine learning algorithms.”
CNN-based models demonstrated superior performance, with reported area under curves (AUCs) ranging from 0.858 to 0.961 and accuracies from 82.3% to 92.6%. Two-stage models that incorporated spatial information fusion showed the highest diagnostic accuracy, while machine learning models using radiomic features showed comparatively lower performance.
The limitations of the study included single-center data, inconsistent imaging protocols, and a lack of external validation, the authors concluded.
You can view the Radboud UMC poster here. The co-authors were Drs. Alma Hoxhaj, Lyanne Molenaar, Antonio Portaluri, Koen Michielsen, Ioannis Sechopoulos, Ritse Mann. You can view the Durham poster here.