CT lung cancer screening is likely to be more cost-effective if it is used to identify other tobacco-related conditions in high-risk people, according to a study published in the Journal of Thoracic Oncology.
The researchers from Canada believe that combining CT screening for multiple conditions with efforts to stop smoking and manage the treatment of heart and lung disease is the key to screening's cost-effectiveness.
Treating patients with lung cancer is expensive, leaving health systems struggling to afford cancer medicines, according to a press release from Elsevier about the study. But diagnosing smoking-related diseases as early as possible could lengthen and improve patients' lives more affordably. There are no national lung cancer screening programs in place because of a lack of evidence that the benefits would outweigh the financial costs.
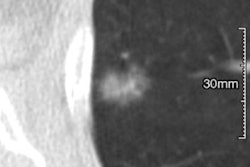
The study showed that large-scale CT lung cancer screening programs could be economically viable if they target high-risk people and are also used to identify noncancer conditions such as chronic obstructive pulmonary disease (COPD) (J Thorac Oncol, May 9, 2017).
"We need to think about how we manage lung cancer and focus on more economically viable strategies, including prevention and screening," said lead author Dr. Sonya Cressman from the Canadian Centre for Applied Research in Cancer Control and the British Columbia Cancer Agency in the release. "Screening those at a high risk gives us the chance to prevent and treat a range of tobacco-related illnesses, and could also offer access to care for individuals who could be otherwise stigmatized or segregated from receiving treatment."
The study examined patient-level data from two major screening trials: the National Lung Screening Trial (NLST) and the Pan-Canadian Early Detection of Lung Cancer Study (PanCan). The researchers built an economic model to simulate the costs and benefits of introducing a CT lung cancer screening program for high-risk people deemed to have at least a 2% chance of developing the disease within six years.
The high-risk subgroup from the NLST was assessed for lung cancer incidence and demographic characteristics compared with those in a low-risk subgroup and PanCan. A decision-analytic model was used to compare high-risk screening versus standard care and determine what would make a screening program most efficient.
By only screening the high-risk individuals, the hypothetical screening program could have reduced the number of people who needed to be screened by 81%, the researchers found. High-risk screening would cost $20,724 (in 2015 Canadian dollars) per quality-adjusted life year gained and would be considered cost-effective at a willingness-to-pay threshold of $100,000 in Canadian dollars per quality-adjusted life year gained. The ability to detect diseases other than cancer was a primary driver of screening's cost-effectiveness, they noted.
Cressman and colleagues also found that the overall cost-effectiveness of the program could be substantially improved if the health of the people being screened were to improve. For example, combining CT screening with smoking cessation and management of cardiac care and COPD would ultimately improve the cost-effectiveness of lung cancer screening.