Quantitative imaging features (QIFs) from FDG-PET combined with conventional prognostic factors of patients with non-small cell lung cancer (NSCLC) show potential to enhance overall survival risk stratification. That's the conclusion of study findings published in the Red Journal and Radiology.
Research is ongoing at the University of Texas MD Anderson Cancer Center to develop models that implement both QIFs and conventional prognostic patient and disease factors, in particular, to help stratify patients with the same disease stage. Patients with the same disease stage typically receive the same treatment for NSCLC, but some may benefit from more aggressive radiotherapy. The use of pretreatment QIFs could aid in the selection and delivery of treatment.
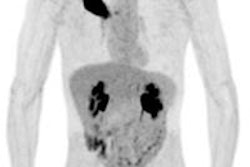
Pretreatment PET is routinely ordered for patients with NSCLC, according to David Fried, lead author and doctoral candidate in MD Anderson's Department of Radiation Physics. Fried and colleagues conducted a study of 195 patients with stage III NSCLC, treated with external-beam radiotherapy during a five-year period commencing January 2008. These patients had a single primary lesion of at least 5 ml in size.
Using 3D reconstructed images from a pretreatment PET scan, the researchers delineated each patient's primary and nodular tumor volumes using semiautomatic software designed for target volume contouring of lung cancer lesions on PET scans. The images and corresponding contours were imported into software developed at MD Anderson that extracts quantitative image features from delineated regions-of-interest. They then used radiology notes and contours from the radiation treatment plan to determine the location of the primary tumor and nodal disease. The contours were used to calculate eight histogram features, four co-occurrence matrix features, and four shape or volume features (International Journal of Radiation Oncology, Biology, and Physics, 29 October 2015 and Radiology, 15 July 2015).
The researchers analyzed 11 conventional prognostic factors including, for example, T and N stage, age, gender, histology, Karnofsky performance status, smoking status, and gross tumor volume. They analyzed 27 QIFs and calculated values for two promising features: the co-occurrence matrix (COM) energy (a metric quantifying the uniformity of standardized uptake value, SUV, within the primary tumor) and disease solidity (the division of the primary and nodal disease volume by the convex hull volume).
Low values of solidity corresponded to dispersed disease, while high values corresponded to disease that was compact and in close proximity. Tumors comprised of homogeneous SUV values had COM energy closer to 1 and those with heterogeneous SUV values had COM energy closer to 0.
Patients were categorized by the radiation dose that they received: 60-70 Gy as low dose and 74 Gy as high dose. To determine whether there was a survival difference between patients who received different radiation doses, each category was then subdivided into groups based on five percentile increments of cut-offs of both solidity and COM energy. The values of the highest 60% of COM energy and 60% of solidity were chosen as a subgroup with a sufficient sample size for analysis.
Patients with high COM energy and high solidity who received a high radiation dose had better progression-free survival and overall survival. No imbalances between groups in terms of conventional prognostic factors were identified. Dose escalation did not benefit patients with low values of COM energy and solidity.
The authors hypothesized that patients with high QIFs, such as compact disease and homogenous FDG uptake, may benefit from dose escalation because they may have a lower incidence and/or severity of toxic side-effects, due to the compact nature of disease and having tumors that are not radio-resistant.
"It is quite apparent that patient survival is contingent upon a multifactorial process and not purely radiation dose," they wrote. "In order to optimize treatment for patients, it would be advantageous to know if certain populations of stage III NSCLC are more likely to benefit from escalating radiation treatment dose ... Additionally, more accurate models could ensure more balanced and/or appropriate treatment arms in prospective trials."
This study may help explain the unexpected results of RTOG 0617, a clinical trial that compared outcomes of patients with unresectable stage III NSCLC who received either high- or low-dose radiotherapy. Survival outcomes were comparable for the 427 participating patients who either received a 60+ Gy or 74 Gy radiation dose.
The authors consider their study to be "hypothesis generating." Their next project is to extract outcome, dosimetric data, and toxicity data to determine whether any trends exist relating to radiation dose and whether QIFs could be useful in better selecting patients for treatment. Additional research is also needed to validate the findings of the study and to determine what factors could be used to select the best radiation dose for an individual patient to maximize his or her survival.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.