
Developing a greater appreciation of the many complications that can occur after shoulder surgery improves interactions between radiologists and orthopedic specialists, according to award-winning work presented at the 2015 congress of the European Society of Musculoskeletal Radiology (ESSR).
Reverse total shoulder arthroplasty is a powerful tool for the treatment of patients with previously unreconstructible shoulder problems and/or failed arthroplasty, noted Dr. Neeraj Purohit, a radiologist at Southampton University Hospital, U.K. Fracture fixation involves the use of plates and intramedullary nails, and building a keen awareness of the various other types of metalwork -- bone anchors and screws -- is essential.
Furthermore, preoperative use of digital x-ray, CT, and MRI can play a valuable role in assessing the bone morphology of the glenoid (version and bone stock) and rotator cuff integrity, explained Purohit, whose e-poster was one of three prize winners singled out by ESSR judges.
Shoulder arthroplasty dates back to 1893, when French surgeon Jules-émile Péan implanted a platinum and rubber prosthesis to replace a shoulder joint that had been destroyed by tuberculosis. In 1951, U.S. physician Dr. Charles Neer developed and pioneered a prosthesis for the management of proximal humeral fractures, and the indications subsequently expanded to include the management of arthritis.
Against this background, Purohit and colleagues elaborated on the current indications and range of implants.
"Degenerative osteoarthritis of the shoulder is less common than in weight-bearing joints," they stated. "As well as osteoarthritis, there are numerous other indications for shoulder arthroplasty: arthritides (degenerative, inflammatory, post-traumatic), severe proximal humeral fractures, shoulder girdle tumors, osteonecrosis, rotator cuff deficiency, revision arthroplasty."
Over the past decade, there has been a rapid increase in the number of shoulder arthroplasty procedures. Hemiarthroplasty, total shoulder arthroplasty, and reverse total shoulder arthroplasty are the three main types of shoulder joint reconstructions requiring prostheses.
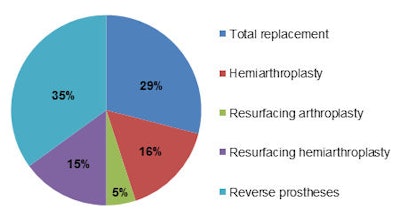 Data from the 2013 U.K. National Joint Registry for primary shoulder arthroplasty.
Data from the 2013 U.K. National Joint Registry for primary shoulder arthroplasty.The U.K. National Joint Registry of 2013 registered a total of 2,225 shoulder replacements, of which 1,968 were primary procedures and 257 were revisions. Of the primary procedures, 29% were total replacements, 16% hemiarthoplasty, 5% resurfacing arthroplasty, 15% resurfacing hemiarthroplasty, and 35% reverse prostheses. The primary diagnosis was osteoarthritis in 58% of cases and cuff arthropathy in 23% of cases.
Other implants that are commonly encountered about the shoulder include devices used in fracture fixation and repair of rotator cuff tendons, including humeral plates and nails, and metallic bone anchors for tendon repair, the authors continued.
"Shoulder arthroplasty can suffer the same fate as hip and knee replacements," they wrote. "Infection, aseptic loosening, and periprosthetic fracture are all complications that can arise around a shoulder prosthesis, with the early signs often being subtle. In cases of fracture fixation, nonunion can be demonstrated on imaging with the patient often necessitating revision surgery."
Familiarization with normal imaging findings in these cases will enable the radiologist to diagnose complications early on and to expedite patient management, they pointed out.
As for preoperative imaging, glenohumeral osteoarthritis leads to posterior glenoid erosion, flattening of humeral head, and rotator cuff tears are uncommon. Not recognizing posterior wear can lead to glenoid component in retroversion and risk posterior instability, according to Purohit et al. CT often is useful in preoperative planning, and particularly for assessments for glenoid version and bone stock. Major wear of the glenoid may require additional bone graft from the humeral head.
Before CT, the glenoid version should be measured on axillary radiographs, they advised. Radiographs have been shown to be ineffective in assessing the glenoid version because of overlapping bones, variation in radiographic technique, and variability and complexity of scapular anatomy. Glenoid version is defined as the angle between a line drawn from the medial border of the scapula to the center of the glenoid, and the line perpendicular to the face of the glenoid on the axial 2D CT slice at or just below the tip of the coracoid.
Scapular neck length is important, especially in reverse total shoulder arthroplasty, because a short neck length can predispose to scapular notching. Studies have shown a scapular neck length of less than 9 mm to be significant, they concluded.
To view the entire ESSR e-poster, click here.



















