Adding ultrasound to mammography screening detects more early invasive breast cancer and probably reduces mortality, according to a 4 November study in the journal Lancet. The Japanese trial is thought to be the first of its kind in a large randomized multicenter population, and that focused on younger women at average risk with dense breast tissue.
The Japan Strategic Anti-Cancer Randomized Trial (J-START) involved the screening of nearly 73,000 women ages 40-49 at 42 study sites across 23 prefectures in Japan. Noriaki Ohuchi, PhD, of Tohoku University in Sendai, Japan, led a team that screened a large cohort of women with ultrasound and mammography, then compared them with women who received only mammography for sensitivity, specificity, and other factors (Lancet, 4 November 2015).
The results were encouraging for breast ultrasound, with 57% more cancers detected in the women who received both modalities. But specificity was lower, and a nagging question remains as to whether the results can be extrapolated to other populations outside of Asia, where rates of dense breast tissue may not be as high.
Mammography's status in Asia
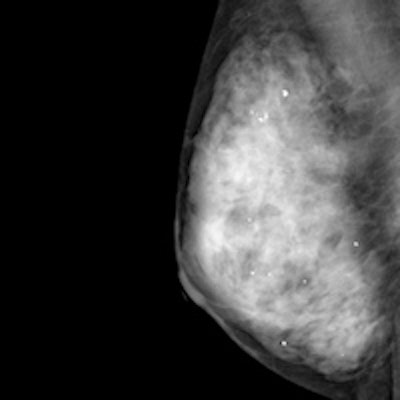
Mammography is the only proven method of screening that reduces mortality, but it is inaccurate in dense breasts, Ohuchi and colleagues wrote. In Asia, where women characteristically have dense breast tissue, age-specific breast cancer incidence peaks in the younger age group of 40 to 49, compared with women 60 to 70 years old in Western countries.
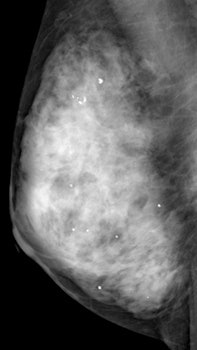 Mammography image of a dense breast. Although mammography is the only proven method of screening that reduces mortality, it is inaccurate in dense breasts, but adjunctive ultrasound can help. Image courtesy of Martin Yaffe, PhD.
Mammography image of a dense breast. Although mammography is the only proven method of screening that reduces mortality, it is inaccurate in dense breasts, but adjunctive ultrasound can help. Image courtesy of Martin Yaffe, PhD.For this study, the researchers started with a population of 72,998 asymptomatic women ages 40-49 at 42 study sites across 23 prefectures in Japan. Eligible women had no history of any cancer in the previous five years and were expected to live for more than five years.
Participants were centrally and randomly assigned to undergo twice in two years either mammography plus ultrasound in the intervention group (36,752 women screened after exclusions), or mammography alone in the control group (35,965 screened after exclusions). The primary outcome was sensitivity, specificity, cancer detection, and stage distribution at the first round of screening.
The study showed that ultrasound combined with mammography resulted in correct identification of cancer in more than nine out of 10 cases for 91.1% sensitivity, compared with 77% sensitivity for women who received mammography alone. In all, 57% more cancers were detected in the intervention group (184 cancers or 0.50%) than in the control group (117 cancers or 0.32%). Further analysis showed that 128 (70%) of 184 cancers detected in the intervention group were invasive, compared with 86 (74%) of 117 in the control group.
Adding ultrasound to mammography also detected more cancers at an early stage: 144 cancers at stage 0-1, compared with 79 cancers at stage 0-1 detected by mammography alone.
The addition of ultrasound also resulted in fewer interval cancers (which appear after a negative test result between scheduled rounds of screening), leading researchers to conclude that adding ultrasound to mammography screening detected additional cancers: 18 (0.05%) interval cancers were detected in the intervention group compared with 35 (0.10%) in the control group.
| Findings | Intervention group participants | Control group participants |
| Participants | 36,752 women | 35,965 women |
| Total cancers that materialized | 202 (0.55%) | 152 (0.42%) |
| Sensitivity | 91.1% | 77% |
| Specificity | 87.7% | 91.4% |
| Cancers detected, of these, invasive | 184 (0.50%) 128 of 184 (70%) |
117 (0.32%) 86 of 117 (74%) |
| Cancers not detected | 18 (0.05%) (8.9% of 202) |
35 (0.10%) (23% of 152) |
| Ultrasound-only detection | 61 (30.2% of 202) 48 stage 0-1 (78.6%) |
-- |
| Cancers stage 0-1 in total cancers | 144 (71.3% of 202 | 79 (51.2% of 152) |
| Further assessment/recall recommended | 4,647 women (12.6%) | 3,153 women (8.8%) |
| Interval cancers, of these, invasive | 18 (0.05%) 16 (89%) |
35 (0.10%) 27 (77%) |
The screening detection rate overall was increased by 0.17% in the intervention group. However, specificity was significantly lower in the intervention group, at 87.7% versus the control group at 91.4%.
The authors believe this problem can be overcome.
"The first reason for low specificity was the separate categorization of the mammographic and ultrasound images, which inevitably led to an increased recall rate and reduced specificity. Combined assessment might improve specificity," Ohuchi et al stated, adding that the recall rate for mammography screening in their study (8.8%) was well within the target range of routine screening mammography (less than 11%).
Further assessment was recommended for more participants (4,647) in the intervention group than in the control group (3,153), and the number of biopsies performed after the first round of screening was also higher in the intervention group. The authors claim sensitivity in the intervention group was higher because of the lower number of interval cancers and because 67 additional cases were detected by ultrasound (and clinical examination). Of these, 55 (82%) were histopathologically invasive. In the intervention group, 48 (78%) of the 61 breast cancers detected by ultrasound alone were clinical stage 0-1, and most were invasive and node negative.
"The difference between the intervention and control groups in the total number of breast cancers detected (202 versus 152) might be explained by the ability of ultrasonography to depict additional cancers, which is supported by our finding of fewer interval cancers in the intervention group (18 versus 35)," Ohuchi et al stated.
The researchers concluded ultrasound could offer a low-cost way to increase sensitivity and detection rates of early cancers in women with dense breasts, but stressed the need for long-term follow-up to assess whether a combined approach could reduce frequency of advanced breast cancers at detection and disease-related mortality.
Ultrasound saves lives
Adjunctive ultrasound can save lives, and hopefully the trial results will lead to further research about the role of ultrasound and its impact on breast cancer screening, noted Martin Yaffe, PhD, professor of medical biophysics and medical imaging at the University of Toronto, in an email to AuntMinnieEurope.com. Modern screening coupled with more effective modern therapies could yield a mortality reduction in the 35% to 45% range, closer to the results seen in modern observational studies, he added.
 Ultrasound can find additional cancers and reduce interval cancer rates. These additional cancers are most likely fast-growing and aggressive, Yaffe points out.
Ultrasound can find additional cancers and reduce interval cancer rates. These additional cancers are most likely fast-growing and aggressive, Yaffe points out."It is reasonable to assume that because the addition of ultrasound to mammography provides increased sensitivity in detecting cancers, some of which are small invasive cancers, there will be a reduction in breast cancer mortality," Yaffe stated. "The magnitude of the effect will depend on the probability that the additional cancers found would have become lethal, and of course we can't be certain about this. But, because the investigators also found that the interval cancer rate was higher in the women not randomized to receive ultrasound, this suggests that at least some of the additional cancers found with ultrasound are the more rapidly growing ones and, therefore, those more likely to be aggressive."
In J-START, follow-up with respect to breast cancer mortality is planned, but it may be more than 10 years before further studies yield meaningful results. However, both Ohuchi et al and Yaffe are clear that ultrasound does help to improve the detectability of small cancers, some of which are invasive.
"We also know from randomized trials, and in observational studies, such as Pan-Canadian Screening Study, published last year, that mammography screening is effective in helping to reduce breast cancer mortality in women over the age of 40. This is despite the fact that many of the younger women have dense breasts where the sensitivity of mammography may be suboptimal," Yaffe noted. "Ultrasound, as a method of improving sensitivity, could be useful in screening these women."
However, the reduction in specificity when ultrasound is added may lead to additional recalls and possibly biopsies of women who do not have breast cancer. The added costs related to additional screening may hamper inclusion of ultrasound in routine screening, Yaffe pointed out. The immediate effect of this trial might be to stimulate further developments in automated ultrasound technology to speed examination and improve specificity, while preserving the gains in cancer detection.
"If screening practice changes in the short term, this will likely occur in Asia, where ultrasound has already made inroads as a screening tool," he wrote.
Until the mortality data are available, however, he believes there will not be strong evidence to support this in other regions. Therefore, it remained important to follow this "average risk" cohort to determine if there is a difference in how many women die due to breast cancer between those who were screened with ultrasound and mammography, versus mammography alone.
"The information on comparative accuracy is already useful. When the mortality data emerges it will be more so," Yaffe concluded.