Digital breast tomosynthesis (DBT) combined with 2D mammography, or synthetic mammography, has better specificity than 2D mammography alone, a large study of more than 7,000 patients has found. However, there was only a marginal improvement in sensitivity.
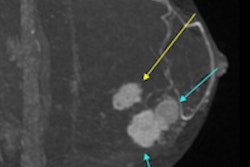
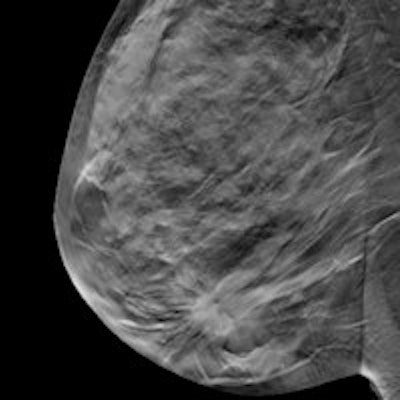
Although mammography is effective at detecting early-stage breast cancer and reducing breast cancer mortality, some cancers are not detected, particularly in women with dense breasts and those younger than age 50. This is often due to overlapping fibroglandular tissue, which can decrease the visibility of abnormalities or mimic abnormalities. The National Health Service (NHS) Breast Screening Program (NHSBSP) finds this cause for concern as it extends the screening to include younger women and women with a family history of breast cancer.
Current evidence indicates DBT should be used as an adjunct to 2D mammography; however, the additional radiation exposure required to obtain a standard 2D mammogram could be avoided if a synthetic 2D mammogram could be reconstructed from the images acquired from DBT imaging.
 Dr. Fiona Gilbert from the University of Cambridge in the U.K.
Dr. Fiona Gilbert from the University of Cambridge in the U.K.
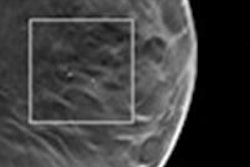
Dr. Fiona Gilbert from the radiology department at the University of Cambridge in the U.K. and colleagues thus compared the diagnostic accuracy of DBT in conjunction with 2D or synthetic 2D, against standard 2D mammography in a retrospective study. They sought to determine if DBT plus 2D or synthetic 2D improves the accuracy of detection of small or subtle breast cancers, cancers in women with dense breasts, cancers presenting as soft-tissue masses, and cancers presenting as microcalcifications, as well as to assess the association of breast density with cancer incidence (Health Technology Assessment, January 2015, Vol. 19:4).
Women from six NHSBSP centers between the ages of 47 and 73 were recalled for further assessment after routine breast screening. Women ages 40 to 49 with a moderate/high risk of developing breast cancer attending annual mammography screening were recruited after giving written informed consent. They all underwent a two-view (mediolateral oblique and craniocaudal) 2D mammogram of both breasts and two-view DBT imaging. Image processing software generated a synthetic 2D mammogram from the DBT datasets.
After exclusions, the 7,060 subjects had 6,020 assessment cases (1,158 cancers) and 1,040 family history screening cases (two cancers). Reading data were available for 6,928 (98%) cases by 2D only, 6,960 (99%) by 2D + DBT, and 6,654 (94%) by synthetic 2D + DBT.
Overall sensitivity:
- 87% for 2D only
- 89% for 2D + DBT
- 88% for synthetic 2D + DBT
The difference in sensitivity between 2D and 2D + DBT was of borderline significance, according to the researchers, but there was no significant difference for synthetic 2D + DBT.
Specificity
- 58% for 2D
- 69% for 2D + DBT
- 71% for synthetic 2D + DBT
Specificity was significantly higher in both DBT reading arms for all subgroups of age, density, and dominant radiological feature, the researchers found. In all reading arms, specificity tended to be lower for microcalcifications and higher for distortion/asymmetry, they added.
| Sensitivity comparison | ||||
| Modality | Invasive tumors 11-20 mm | 50% or more breast density | Grade 2 invasive tumors | Mass as dominant radiological feature |
| 2D + DBT | 93% | 93% | 91% | 92% |
| 2D alone | 86% | 86% | 87% | 89% |
For synthetic 2D + DBT, the researchers found a significantly higher sensitivity than 2D alone in invasive cancers 11 mm to 20 mm in size, with a sensitivity of 91%.
Although the study was in agreement with recent published studies demonstrating that 2D plus DBT performed better than 2D alone in terms of specificity, the researchers were unable to demonstrate the same significant increase in sensitivity for 2D plus DBT reported in those studies.
"Our study design clearly limits estimation of the impact of DBT on diagnostic performance and extrapolation of our results to a screening population," the researchers wrote. "Our method of case selection of index test cases meant that the relative benefit of DBT on sensitivity has been underestimated, since these cases have already been detected by 2D screening. Similarly, this dataset is likely to have overestimated the impact of DBT on specificity."
Because 2D plus DBT imaging was shown to be more effective than 2D alone across all age groups and breast densities, it would be advantageous to the planned age extension of the NHSBSP for younger women who have denser breast tissue and those with a family history of breast cancer.
"The potential of combined 2D + DBT imaging to reduce the burden of false-positive recalls and associated diagnostic assessments would also benefit screening programs," Gilbert and colleagues wrote. "Although this study was not designed to assess DBT in the diagnostic and assessment setting, improved visualization of benign and malignant features using DBT could reduce the need for additional ultrasound, MRI, or supplemental mammographic imaging. The screening population would also benefit if some of the anxiety and stress associated with breast screening from unnecessary recalls and additional testing could be reduced."
Combined 2D plus DBT imaging has been approved for screening in the U.S., but cautiously. In July 2014, the American College of Radiology (ACR) stated: "While there is strong evidence that tomosynthesis will have an important role in breast imaging, further studies are needed to assess tomosynthesis' relationship to long-term clinical outcomes, including reduced mortality. It will also be important to learn which subgroups of women might benefit most from these exams."
Gilbert and colleagues contend that, while additional information on the performance of DBT is required, the accepted "gold standard" of a randomized controlled trial comparing 2D and 2D + DBT would be time-consuming and expensive, and it could "delay implementation of a key imaging technology in screening by five to seven years."
Because no formal cost-effectiveness/cost-benefit evaluations have been published, they suggest the feasibility and practicalities of implementing DBT into the workflow of a U.K. screening setting should be evaluated, which would include a cost-effectiveness evaluation or modelling. It would also include evaluation of the additional costs (e.g., upgrading equipment), providing information technology support for image archiving, connectivity to PACS and IT systems, increased reading time, and potential benefits (e.g., increased cancer detection, particularly small invasive cancers, reductions in false-positive recalls, additional diagnostic testing, and reduction in interval cancers).
The study authors have several recommendations for future research, such as following:
- Comparative work with synthetic 2D and 2D alone; for example, quantifying the effect on sensitivity and specificity for lesions with different radiological appearances, of different pathological types (e.g., DCIS, invasive, different grades of tumor) and in different types of breast (e.g., more than 50% density)
- Screening studies with DBT systems other than Hologic's, which could be partly achieved by modeling using simulated lesions and observer studies such as OPTIMAM (optimization of breast cancer detection using digital radiograph technology)
- Comparison with 2D on the size, grade, and type of cancers detected by DBT, for interval cancers and for cancers detected in the subsequent screening round, where the same degree of improvement in the detection of invasive cancers would not be expected
- Prognostic modeling on existing datasets of screen-detected and interval cancers to predict the outcome of cases and projected impact on breast cancer mortality, which could be achieved using, for example, the Nottingham Prognostic Index.
- DBT's ability to discriminate between early aggressive cancers and slow-growing DCIS to address any concerns about DBT contributing to overdiagnosis
Declared competing interests of authors: Dr. Michell reports personal fees, nonfinancial support and grants from Hologic, the supplier of the mammographic and tomographic equipment, outside the submitted work. Dr. Astley reports grants from National Institute for Health Research (NIHR) during the conduct of the study; nonfinancial support from Matakina; and workshop training sessions and nonfinancial support from Hologic outside the submitted work. No others declared.