For the second time since 2013, the Olbert Interventional Radiological Symposium (IROS) will be held this week in Berlin, from 15 to 17 January. This is the biggest conference for minimally invasive and computer-guided therapy in the German-speaking world and will bring together nearly 1,000 specialists to discuss the latest trends in this growing discipline. The congress president, Dr. Markus Düx, professor and head of radiology at the Nordwest Hospital in Frankfurt am Main, explains about the principal themes.
The German Radiological Society (DRG): The focus of IROS 2015 is interventional pain therapy. For which patients is it used?
 Dr. Markus Düx.
Dr. Markus Düx.Düx: The spectrum is very wide. Starting with the treatment of painful degenerative bone diseases, such as painful tendon attachment points or painful facet joints, it encompasses patients with prolapsed intervertebral disks and extends as far as the treatment of bone tumors and soft tissue.
Sometimes all that is needed to abolish or alleviate the pain is an injection of long-acting analgesics and cortisone at the site of the pain. Of course, other specialists also do this. However, the advantage of treatment from radiologists is that they use modern image guidance and therefore are best able to navigate within the body so that the site of the pain can actually be reached.
What is the role of interventional radiology in tumor pain?
Tumor patients are a sensitive and highly specific group. The pain is usually very severe, cannot be controlled by analgesics, and is inaccessible to other procedures, so this is where interventional radiology comes in. With painful osteolytic processes, such as, for instance, bone metastases, we can carry out cementation and stabilization using minimally invasive access or we can destroy the tumor locally with CT-guided probes inserted into a painful area of tumor, and this is called ablation.
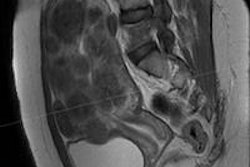
 Painful osteoblastic prostate cancer metastasis in the right ilium (arrow). All images copyright of Dr. Markus Düx.
Painful osteoblastic prostate cancer metastasis in the right ilium (arrow). All images copyright of Dr. Markus Düx.The most common procedure is thermal ablation, which "cooks" the tumor tissue. Thermal ablation can be used even with large tumors because it treats only that part of the tumor which is causing the pain. The effect is the patient is no longer aware of the pain, even if the thermal ablation cannot destroy the entire tumor.
Some methods allow totally noninvasive treatment. This is the latest trend: intervention without needles or catheters in, for instance, the treatment of uterine fibroids. These benign uterine tumors can be treated with focused ultrasound (FUS). The ultrasound waves are concentrated to produce heat within a focal point. To treat uterine fibroids, the ultrasound waves are applied via an ultrasound source in the MRI table, MRI being used as an imaging procedure to locate the fibroids and to measure the development of the temperature within the fibroid and surrounding tissues during treatment.
 Noninvasive thermal ablation of a prostate cancer metastasis, using focused ultrasound, entirely without needles, catheter, or scalpel. The area highlighted in blue shows the heat distribution within the bone and tumor, which is measured with the aid of MRI during treatment and that ultimately displays the destruction of the metastasis.
Noninvasive thermal ablation of a prostate cancer metastasis, using focused ultrasound, entirely without needles, catheter, or scalpel. The area highlighted in blue shows the heat distribution within the bone and tumor, which is measured with the aid of MRI during treatment and that ultimately displays the destruction of the metastasis.Many affected women, whose only prospect once was the removal of the uterus or surgical removal of the fibroids, have since been treated successfully with this method, with the uterus being preserved.
And now we've come back to pain therapy! FUS is also effective against severe back pain and painful bone metastases. In painful facet joint arthritis, FUS desensitizes the nerve that transmits pain at the zygapophyseal joint; this means that the sense of pain is switched off, while the other functions of the nerve are preserved.
 Pleural carcinosis in ovarian cancer with severe intercostal neuralgia due to tumor compression at the nerve exit point (arrow).
Pleural carcinosis in ovarian cancer with severe intercostal neuralgia due to tumor compression at the nerve exit point (arrow).The remarkable thing about focused noninvasive ultrasound is the immediate and lasting abolition or alleviation of pain. If, however, the pain recurs later, the FUS treatment can be repeated.
Interventional radiology is also becoming increasingly popular with hospital managers. No wonder. The minimally invasive treatments given by radiologists shorten the length of hospital stays. Many procedures can actually be offered on an entirely outpatient basis, and the staffing and surgical costs are also much lower than with many "major surgery" procedures. However, the patient's welfare is central. And here we see, besides therapeutic success, much lower complication rates and a shorter recovery time.
 Treating pain by introducing a probe into the tumor under CT guidance. The tip of the probe (arrow) is heated to 100°C with the aid of microwave energy and leads to thermal ablation of the tumor tissue with immediate relief from pain.
Treating pain by introducing a probe into the tumor under CT guidance. The tip of the probe (arrow) is heated to 100°C with the aid of microwave energy and leads to thermal ablation of the tumor tissue with immediate relief from pain.How is the quality of treatment assured?
This is an important point. The methods are no longer "niche;" they are used for many patients and in many facilities. Also, there is an enormous innovative push; new minimally invasive techniques or refinements of existing techniques are constantly emerging. This means the specialist organizations are faced with the important task of quality control, e.g., by means of structured continuing education, as offered at the IROS.
For several years now, there has been a certification scheme for interventional radiology and neuroradiology, which is open to specialist radiologists and gives solid quality controlled documentation for the individual categories -- such as minimally invasive pain therapy, tumor therapy, and the minimally invasive treatment of vascular disease. A work-shadowing network is also being established. It offers young colleagues on-the-job training, under the direction of experienced interventionists.
For more information about the congress of the German, Austrian, and Swiss societies for interventional radiology (DeGIR, ÖGIR, and SSCVIR), click here.
Editor's note: This is an edited version of a translation of an article published online on 6 January 2015 in German by the German Radiology Society (DRG). Translation by Syntacta Translation & Interpreting.