Oncologists need more information from radiologists to improve assessment of treatment response, and 3D volumetry techniques can be ideal for this purpose, yielding precise and invaluable prognostic information such as early tumor shrinkage, according to Dr. Anno Graser, head of oncologic imaging at the University of Munich.
Furthermore, semiautomated volumetry methods are reproducible and can reduce misclassification of therapy treatment response, offering an improvement over the less-than-exact Response Evaluation Criteria in Solid Tumors (RECIST)-based estimates of tumor volume, Graser said.
"Radiologists need to provide volumetry to keep with requests [from oncologists], for example, [about] early tumor shrinkage," he said.
Graser spoke during a presentation at the recent International Symposium on Multidetector-Row CT in Washington, D.C.
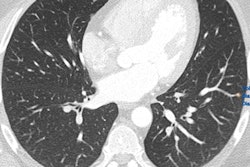
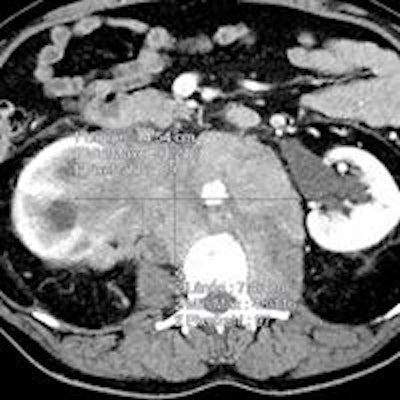
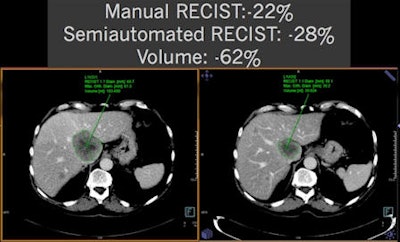
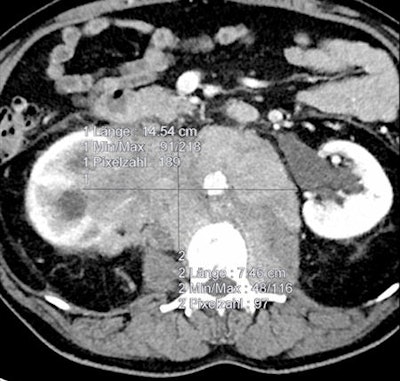 As shown in these cases, volumetry is more sensitive than RECIST measurements for determining therapy treatment response. All images courtesy of Dr. Anno Graser.
As shown in these cases, volumetry is more sensitive than RECIST measurements for determining therapy treatment response. All images courtesy of Dr. Anno Graser.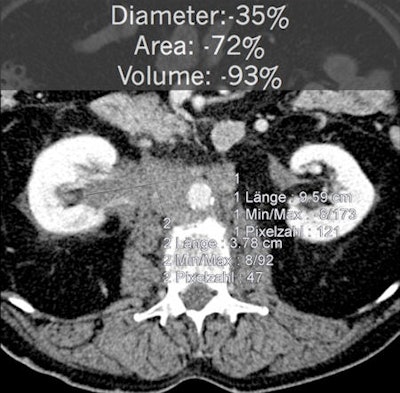
In the majority of metastatic cancer patients, imaging is by far the most important biomarker to monitor response to treatment, Graser said.
"Without [radiologists], the oncologists really don't know what's going on in their patients," he said.
In addition, accuracy in imaging of treatment response is even more important given the increasing cost of treatment. Response assessment measures on imaging include tumor size, density, and volume. There's evidence that volumetry can more exactly quantify early tumor shrinkage, however, Graser said.
Why should radiologists consider volumetric assessments? "Our oncologic colleagues want us to get better and want us to provide them with new information," he said.
Early tumor shrinkage
In patient data from the CRYSTAL metastatic colorectal treatment trial, RECIST measurements showed early tumor shrinkage of 15.4%. But volumetry revealed early tumor shrinkage of 61.5%, Graser said.
The importance of early tumor shrinkage is a hot topic in radiation oncology today, Graser said. In the CRYSTAL and OPUS metastatic colorectal cancer treatment trials, progression-free survival was significantly higher in patients with early tumor shrinkage by more than 20% at first reassessment than those with less than 20% early tumor shrinkage (Acta Oncologica, June 2012, Vol. 52:5, pp. 956-962).
"This also translates into a prolonged overall survival, so somehow this seems to be a very important biomarker," Graser said. "This data was generated using RECIST measurements only; imagine what would happen if you did the same thing with volumetry."
Radiologists will have to provide this data to keep up with the amount of information that oncology wants, he stressed. Looking at data in the CRYSTAL and OPUS trials even more closely, progression-free survival and overall survival differed significantly with early tumor shrinkages, but only for KRAS Wild-Type patients. KRAS Mutant patients had no significant difference in progression-free survival and overall survival based on early tumor shrinkage.
"We as radiologists need to know about new markers and we need to know about new histopathology and other markers that we really didn't think about so much," Graser said. "We're all aiming at what they call individualized tumor profiling."
The degree of early tumor shrinkage can be used to predict patient outcome and progression-free survival, and can be calculated via simple measurements without the need for an extra scan, he said.
Automated tumor volumetry?
In an attempt to determine whether automated tumor volumetry was necessary or if tumor lesion volume estimates were sufficient, researchers studied 20 patients as part of the two-armed, randomized, phase II multicenter CIOX trial on metastatic colorectal cancer.
In these 20 patients there were a total of 151 target lesions, including:
- Liver: 137 (90.7%)
- Lung: Four (2.6%)
- Lymph node: Six (4%)
- Abdominal wall: Two (1.3%)
- Adrenal gland: Two (1.3%)
Semiautomated volumetry using a commercially available system and manual measurements of the longest RECIST 1.1 diameter and longest orthogonal diameter were performed. When comparing the manual measurements, the researchers found that simulating volume by extrapolating RECIST-based measurements would systematically overestimate tumor volume. However, volume simulations would be relatively accurate based on the World Health Organization (WHO) tumor burden criteria, Graser said.
In a recent multicenter evaluation of manual versus semiautomated measurements of tumor volume in lymphoma patients, researchers studied 59 patients with malignant lymphoma. The patients had 290 lymph nodes (5 ± 2 per patient) measured at baseline and follow-up (after two cycles of chemotherapy).
Manual measurements were performed at five German university hospitals for long axis diameter, short axis diameter, and WHO area. Semiautomated measurements of the same parameters and volume were also performed.
Manual measurements took an average of 16.6 ± 13.3 seconds to produce. In the 41.9% of semiautomated measurements that were performed without needing corrections, volumetry took an average of 13.7 ± 7 seconds. However, volumetry required an average of 48.4 ± 30.2 seconds for the 58.1% of cases that needed manual correction. Taking into account all cases, volumetry was performed in an average time of 33.8 ± 29.0 seconds, twice as long as manual measurements.
Volumetry does offer advantages, however, Graser said.
"If you look at a new criteria like 'excellent response,' which is defined as volume reduction of more than 50%, you can now classify the patients as very good responders, as opposed to partial response, stable disease, and progressive disease," he said.
In the multicenter study, manual WHO area calculations had a relative standard deviation of 19.2% and a standard deviation of 18.5%, while the semiautomated calculations had a relative standard deviation of 9.8% and standard deviation of 11%, Graser said.
The automated method also reduced misclassification of therapy response across all centers.
| Manual | Automated | |
| Correct | 44% [range: 34-48%] | 60% [range: 55-66%] |
| Incorrect | 56% [range: 52-66%] | 40% [range: 34-45%] |
"I guess we still don't know whether volumetry can be called better than RECIST, but we have seen that semiautomated measurements are more reproducible," Graser concluded. "RECIST-based estimates of volumes are not exact, so we need to really measure and segment."