Used properly, MRI is a sensitive, specific, safe, and reliable tool for evaluating Crohn's disease activity and complications, and is useful for assessing the extent and severity of the disease, according to gastrointestinal specialists from the U.K.
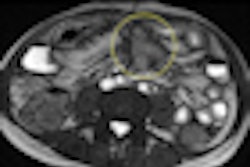
"It is relatively less sensitive in making diagnosis in early mucosal disease. It is essential to assess this prior to use of powerful immunosuppressive therapies. Extramural complications like abscess formation is of particular importance while considering immunosuppression," noted Dr. V. Chidambaram and Dr. A.D.C. Jacob, from the department of imaging at the University Hospital of North Staffordshire NHS Trust, Stoke-on-Trent. "Endoscopy is the gold standard. But limited information is provided in assessment for extraluminal complications, distribution, accessing segments beyond strictures."
CT continues to play a role in acutely unwell patients, they told attendees at the 2012 meeting of the European Society of Gastrointestinal and Abdominal Radiology (ESGAR). Enteroclysis can be useful, but is cumbersome and involves radiation for nasojejunal tube placement. In most instances, enterography is adequate, they said.
At their department, MRI examinations are conducted on a 1.5-tesla Siemens Healthcare system. Patients are asked to drink Klean Prep (macrogol-based, 69g sachet from Norgine). The preparation is mixed in a liter of water and taken over 90 minutes. The exam takes between 40 and 60 minutes, and 10 mg of Buscopan is given beforehand. Patients are investigated in the prone position, unless they have a stoma or fistula, or cannot lie prone. Prone scanning reduces compression of the abdomen, therefore reducing the number of slices and enabling faster scanning and better breath-holds, the researchers noted.
They use initial reference localizers for planning the investigation. In addition, they use 6 mm coronal fast imaging with steady-state precession (FISP) sequences to check contrast has reached the colon and assess distension; if it has not done so, they ask the patient to continue taking the oral contrast, and they wait for about 15 to 20 minutes.
"Adequate distension needs to be achieved or spurious wall thickening and other inferences can be made or missed. Artifacts from luminal flow can mimic fold abnormalities, therefore Buscopan should be used," they noted, adding that a subjective decision must be made about enhancement patterns and newer objective measures with enhancement curves are currently in research and are coming into fashion.
Because early disease remains difficult to diagnose consistently, MRI plays a central role in assessing disease extent and severity in a patient with known Crohn's disease rather than in primary diagnosis. It remains the modality of choice in follow-up, and typically in disease relapse, suspected structuring disease, extraluminal complication, treatment failure, and surgical planning, they stated.
"Fistulation is best assessed on a more dynamic imaging. This is currently best provided by fluoroscopy. When in doubt or when surgical planning requires, fluoroscopy should be used," the researchers pointed out. "Colon assessment is poor especially when there is significant fecal residue and assessment should be made with caution."
Bowel wall fat deposition can occur in normal and obese patients, similarly structuring can be due to many causes. Differentials should be kept in mind while assessing cases, they advised.
Overall, MRI remains expensive and some patients do not tolerate it, and shorter sequences with limited breath-holds are helpful, Chidambaram and Jacob concluded.