A 12-year audit conducted at a women’s imaging facility in Australia has provided new data on the link between mammographic breast density and breast cancer detection.
“Breast density is increasingly recognized worldwide as an independent risk factor for breast cancer,” noted Dr. Ben Trinh, a radiology registrar in the Department of Health (WA Health) in Perth, and radiologist Dr. Vanessa Atienza-Hipolito, clinical director and owner of Women’s & Breast Imaging (WBI), Cottesloe and Murdoch, and founder of V Imaging in Murdoch, Western Australia. “The Royal Australian and New Zealand College of Radiologists (RANZCR) recently updated their position statement to recommend breast density reporting in all mammographic assessments.”
Understanding this relationship in women under the age of 50 is relevant to both clinical and policy discussions, especially within diagnostic centers managing both symptomatic and asymptomatic referrals, they pointed out.
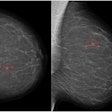
 Correlative mammographic, sonographic, and histopathological findings in a 44-year-old woman with a palpable right breast lump. Synthesised 2D mammogram, right breast, mediolateral oblique (MLO) projection: No discrete abnormality is visualised. Interpretation is limited by heterogeneously dense parenchyma (density grade C). All figures courtesy of Dr. Ben Trinh, Dr. Vanessa Atienza-Hipolito, Women’s & Breast Imaging, presented at RANZCR 2025.
Correlative mammographic, sonographic, and histopathological findings in a 44-year-old woman with a palpable right breast lump. Synthesised 2D mammogram, right breast, mediolateral oblique (MLO) projection: No discrete abnormality is visualised. Interpretation is limited by heterogeneously dense parenchyma (density grade C). All figures courtesy of Dr. Ben Trinh, Dr. Vanessa Atienza-Hipolito, Women’s & Breast Imaging, presented at RANZCR 2025.
 Synthesized 2D mammogram, right breast, craniocaudal (CC) projection of the same patient. No mammographic abnormality is identified. Dense fibroglandular tissue (density grade C) reduces sensitivity.
Synthesized 2D mammogram, right breast, craniocaudal (CC) projection of the same patient. No mammographic abnormality is identified. Dense fibroglandular tissue (density grade C) reduces sensitivity.
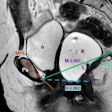
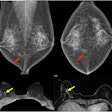
 Right breast, 11 o’clock position, same patient. An 11 mm irregular hypoechoic solid lesion with microlobulated margins, ductal extension, adjacent fat plane distortion, and internal vascularity on Doppler. This corresponds to the palpable abnormality. Biopsy confirmed invasive ductal carcinoma, Grade 2, ER positive, PR positive, HER2 positive, concordant with imaging findings.
Right breast, 11 o’clock position, same patient. An 11 mm irregular hypoechoic solid lesion with microlobulated margins, ductal extension, adjacent fat plane distortion, and internal vascularity on Doppler. This corresponds to the palpable abnormality. Biopsy confirmed invasive ductal carcinoma, Grade 2, ER positive, PR positive, HER2 positive, concordant with imaging findings.
 Right breast, 10 o’clock position, same patient: A 15 mm irregular hypoechoic solid lesion with suspicious morphology, situated approximately 6 mm from the index lesion. Biopsy confirmed invasive ductal carcinoma, Grade 2, ER positive, PR positive, HER2 positive, concordant with ultrasound features. Findings are in keeping with multifocal invasive ductal carcinoma in a heterogeneously dense breast. The patient was referred for surgical management.
Right breast, 10 o’clock position, same patient: A 15 mm irregular hypoechoic solid lesion with suspicious morphology, situated approximately 6 mm from the index lesion. Biopsy confirmed invasive ductal carcinoma, Grade 2, ER positive, PR positive, HER2 positive, concordant with ultrasound features. Findings are in keeping with multifocal invasive ductal carcinoma in a heterogeneously dense breast. The patient was referred for surgical management.
Breast density is determined by many factors, including genetics, age, body mass index, pregnancy, hormone replacement therapy, and age of menarche and menopause. Women with dense breast tissue have more glandular tissue compared to fatty tissue. Breast density is determined by mammography and, therefore, it must not be described by clinical examination, the researchers explained.
“Studies have shown that women with extremely dense breasts are at approximately two-fold increased risk of breast cancer compared to others,” they stated at the annual scientific meeting (ASM) of the RANZCR. “The sensitivity of mammography is reduced in dense breasts, and supplemental investigation with tomosynthesis, ultrasound, contrast-enhanced mammography, and MRI is often required.”
Trinh and Atienza-Hipolito conducted a retrospective single-center audit at a mixed diagnostic center (2013–2024) to assess the correlation between mammographic breast density and breast cancer detection in women between the ages of 40 and 49. Data on demographics, mammographic breast density, and cancer type were retrieved from internal records. Automated volumetric software categorized breast density (A/B = nondense; C/D = dense). Cases with missing density data were excluded.
Approval from the Formal Human Research Ethics Committee (HREC) was not required as this work constituted a retrospective audit/quality improvement activity, they noted.
Of the sample of 199 women, 34 lacked density data and were excluded, leaving 165 cases. Distribution was as follows: A (almost entirely fatty) = 4 (2.4%); B (scattered) = 26 (15.8%); C (heterogeneously dense) = 54 (32.7%); D (extremely dense) = 81 (49.1%).
A high proportion (82%) of women ages 40 to 49 diagnosed with breast cancer in this cohort had dense or extremely dense breasts, the researchers said. “These findings are consistent with international data indicating that mammographic density is an independent risk factor for breast cancer. While mammography remains the primary diagnostic tool, adjunctive imaging may be considered on an individualized basis.”
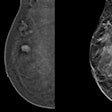
 Correlative tomosynthesis, sonographic, and histopathological findings in a 45-year-old woman presenting with a palpable right breast lump. Synthesized 2D mammogram, right breast, mediolateral oblique (MLO) projection. No discrete abnormality is visualized due to extremely dense parenchyma (BI-RADS category D). A retroglandular silicone breast implant is in situ.
Correlative tomosynthesis, sonographic, and histopathological findings in a 45-year-old woman presenting with a palpable right breast lump. Synthesized 2D mammogram, right breast, mediolateral oblique (MLO) projection. No discrete abnormality is visualized due to extremely dense parenchyma (BI-RADS category D). A retroglandular silicone breast implant is in situ.
 Synthesized 2D mammogram, right breast, craniocaudal (CC) projection of the same patient. No mammographic abnormality is seen. Sensitivity is markedly reduced by dense breast tissue. A retroglandular silicone breast implant is present.
Synthesized 2D mammogram, right breast, craniocaudal (CC) projection of the same patient. No mammographic abnormality is seen. Sensitivity is markedly reduced by dense breast tissue. A retroglandular silicone breast implant is present.
 3D breast tomosynthesis, right breast, MLO push-back view of the same patient. Localized increased stromal density corresponding to the clinically palpable lump, more evident compared with routine 2D projections.
3D breast tomosynthesis, right breast, MLO push-back view of the same patient. Localized increased stromal density corresponding to the clinically palpable lump, more evident compared with routine 2D projections.
 3D breast tomosynthesis, right breast, CC push-back view of the same patient. No definite abnormality demonstrated due to extremely dense breast parenchyma, underscoring the masking effect of density.
3D breast tomosynthesis, right breast, CC push-back view of the same patient. No definite abnormality demonstrated due to extremely dense breast parenchyma, underscoring the masking effect of density.
 Whole breast ultrasound (selected image), right breast, 10 o’clock position, same patient. An 8 mm irregular isoechoic solid lesion with microlobulated margin, ductal extension, and adjacent fat plane distortion. The lesion is sonographically suspicious and correlates with the palpable abnormality and tomosynthesis findings. A retroglandular silicone breast implant is noted, intact. Biopsy confirmed invasive ductal carcinoma, Grade 1, ER positive, PR positive, HER2 equivocal (2+). Low-grade ductal carcinoma in situ with solid architecture was also identified. Findings are consistent with invasive ductal carcinoma in an extremely dense breast. The patient was referred for surgical management.
Whole breast ultrasound (selected image), right breast, 10 o’clock position, same patient. An 8 mm irregular isoechoic solid lesion with microlobulated margin, ductal extension, and adjacent fat plane distortion. The lesion is sonographically suspicious and correlates with the palpable abnormality and tomosynthesis findings. A retroglandular silicone breast implant is noted, intact. Biopsy confirmed invasive ductal carcinoma, Grade 1, ER positive, PR positive, HER2 equivocal (2+). Low-grade ductal carcinoma in situ with solid architecture was also identified. Findings are consistent with invasive ductal carcinoma in an extremely dense breast. The patient was referred for surgical management.
Multicenter and population-based studies are now necessary to further assess density-related cancer detection in younger women, they stated. “This work could inform ongoing discussions within BreastScreen Australia and RANZCR regarding risk-tailored strategies.”
Because this was a retrospective, single-center audit in a diagnostic setting, the findings may not be generalizable to population-based screening. Also, missing density data limited the analysis, the authors added.
To read the full poster, click here.