Global prostate MRI acquisition parameters continue to vary widely around the world, researchers from a leading U.K. facility have reported.
The variations are not good news for quality patient care, wrote a team led by Dr. Francesco Giganti, PhD, of the University College London Hospital NHS Foundation Trust, in an article posted on 10 October by Genitourinary Imaging.
"The introduction of MRI into international guideline recommendations for prostate cancer diagnosis has led to a steep increase in the demand and use of this technique over the past few years," the authors noted. "However, a major concern about more widespread use of this technology is its ability to produce high-quality images with the existing healthcare infrastructure."
Poor MRI quality can influence the ability to diagnose and treat prostate cancer, and concerns have been raised over whether results seen with level I evidence studies are reproducible in typical centers that perform prostate MRI, they added.
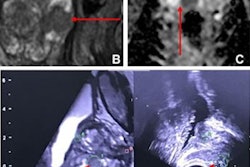
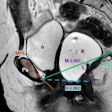
Giganti's team sought to assess the quality of MRI scanners included in the quality control phase of the global Prostate Imaging Using MRI ± Contrast Enhancement (PRIME) trial using the Prostate Imaging Quality (PI-QUAL) standardized scoring system.
In phase I of the study, 41 centers from 18 countries submitted five consecutive prostate studies for each MRI scanner (total, 355 exams from 71 scanners) and a description of the MRI protocol used. Between September 2021 and August 2022, two genitourinary radiologists evaluated these data using the PI-QUAL metric, which is based on a five-point scoring system (scores of 1 and 2 are considered nondiagnostic; 3 is considered sufficient; 4 is considered adequate; and 5 is considered optimal).
Phase II of the study included 48 centers that did not achieve a PI-QUAL 5 score and were invited to resubmit new MR imaging data using a recommended protocol.
The team found the following in phase I:
- 13% of scanners achieved a PI-QUAL score of 3.
- 55% achieved a score of 4.
- 32% achieved a score of 5.
In the phase II part of the research, the group found:
- 92% of dynamic contrast-enhanced sequences did not adhere to PI-QUAL system criteria, followed by 42% of diffusion-weighted imaging sequences and 40% of T2-weighted sequences.
- 36 centers from 17 countries resubmitted revised prostate MR exams; of these, 97% had a final PI-QUAL score of 5.
"Despite initial MRI quality being fair, there was room for improvement, particularly with dynamic contrast-enhanced imaging," the researchers concluded. "With basic changes in line with the Prostate Imaging Reporting and Data System technical recommendations and by using a standardized scoring system such as Prostate Imaging Quality (and its future iterations), global MRI quality can be easily improved."
The complete study can be found here.