VIENNA - Adding dense breasts as a new standard indication for MR mammography in cases with unclear findings could ward off approximately 88% of biopsies and end up saving insurance companies money, according to research presented on Sunday morning at ECR 2013.
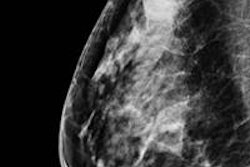
According to the American College of Radiology (ACR) guidelines, the standard indications for MR mammography are status after operation, radiotherapy, previous breast cancer, a high-risk patient, and cancer unknown primary syndrome. Dr. Clemens Kaiser, from the Institute of Clinical Radiology and Nuclear Medicine at the University of Mannheim in Germany, and colleagues added a new indication: dense breasts.
In an agreement with one of the major German insurance companies, unclear findings in other modalities such as x-ray and ultrasound were referred to the clinic for breast MR.
"In these cases, a biopsy would have been the inevitable next step," Kaiser said.
The study included 1,488 patients evaluated between April 2006 and September 2011. Of these patients, 142 were referred to biopsy, 124 because the MR findings detected something suspicious. Eighteen received a biopsy "even though they were MR negative [because] the surgical breast specialist demanded the biopsy," Kaiser said. "They turned out to be negative, though."
More than 1,300 patients didn't receive a biopsy, but they were subject to follow-up or the researchers tried to reach the patients by letter to get some information about their health status.
Close to 400 letters were sent and information was received from 192 patients. The researchers inquired about health status with questions such as: "Are you OK? Did you have any surgery in the breast? How are you doing?"
There were 90 suspected cancer cases, of which 63 were histologically proved and 27 turned out to be benign. There were 34 suspected ductal carcinoma in situ (DCIS) cases, of which 13 were histologically proved and 21 were benign.
There were 76 true positives, 48 false positives, 971 true negatives, and no false negatives. "That means we had a sensitivity of 100% and specificity of 95.2%," he said.
Positive predictive value (PPV) was 61.3% and negative predictive value (NPV) was 100%, with an accuracy of 95.6%, according to the researchers.
"When we take a look at the cancer cases only, DCIS is a different topic," he said. There were 63 true positives, 27 false positives, 971 true negatives, and zero false negatives.
"That left us with a sensitivity of 100% for invasive cancers, a specificity of 97.2%, PPV of 70%, an NPV of 100%, and an accuracy of 97.5%," he said. "That means when you consider that biopsy would have been the inevitable consequence for most of these patients, we were able to prevent at least 88.7% of biopsies with all the financial, psychological, and medical consequences."
Kaiser concluded that dense breasts are indeed an indication for MR and it is suited to solving diagnostic problems. However, the results are strongly dependent on reader experience and adequate technical standards as prerequisites for optimal diagnosis, he said.
"We definitely have to update our BI-RADS lexicon and think about in the future whether [MR is] a problem solver," he said. "There are so many financial aspects in either direction and a consequence is that we know ... when you use MR you don't need ultrasound or mammography. So that might be the future. It's definitely not the case today. But I hope we'll move in this direction."
An audience member pointed out that MR is not a cheap option.
"There is cost and price," Kaiser said. "There are so many things to think about. It's also about early detection of cancer, it's also about saving money in chemotherapy, it's also about money for radiation, and all of that. That adds up to a lot of money the insurance company might be saving."
Kaiser and his colleagues will publish a paper about the economic aspects of their study in the future.