Ultrasound has an edge in sensitivity over digital breast tomosynthesis (DBT) as an accompaniment to standard 2D mammography in women with dense breast tissue. But better sensitivity may not be enough to make ultrasound the gold standard for these women, according to a study presented at the European Breast Cancer Conference, sponsored by the European Cancer Organization (ECCO).
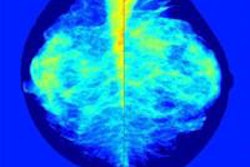
Tomosynthesis may still be the more promising modality for breast cancer screening even though ultrasound detects more cancers, said presenter Dr. Nehmat Houssami, PhD, of the University of Sydney in Australia. Why? Because tomosynthesis can be easily incorporated into standard 2D mammography protocols, while finding 50% of mammographically occult breast cancers.
"In [our] study we are comparing two additional tests to see if they can do better than standard mammograms in finding cancer in women with dense breasts," she said in a statement released by ECCO for the conference this week in Amsterdam. "We have found that ultrasound does better than tomosynthesis, but ultrasound is a separate test, it is time-consuming, and in less experienced hands it can lead to a lot of false alarms. However, tomosynthesis, which is a form of refined mammography, can be carried out as part of the standard 2D mammogram screen, or even instead of it."
Prepare to be ... astounded?
The data Houssami reported are interim results from the Adjunct Screening with Tomosynthesis or Ultrasound in Mammography-Negative Dense Breasts (ASTOUND) trial, led by Dr. Alberto Tagliafico of the University of Genoa in Italy. The trial began in 2012, with the purpose of comparing the cancer detection capability of tomosynthesis versus ultrasound in women with dense breasts. In addition to being presented at the conference, the results were published online in the Journal of Clinical Oncology (March 9, 2016).
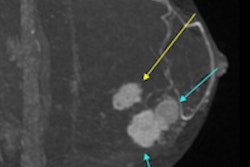
Houssami and colleagues analyzed data from 3,231 women who had negative mammograms but whose breast tissue was categorized as BI-RADS 3 or 4. The women also underwent tomosynthesis and ultrasound exams. Their 2D and tomosynthesis exams were read by the same radiologist; the ultrasound exams were interpreted by a different radiologist, who was blinded to the tomosynthesis images but aware that the mammogram was negative.
The two additional modalities found 24 breast cancers that 2D mammography had missed. Tomosynthesis identified 13 of these, for a detection rate of four cancers per 1,000 screening exams, while ultrasound identified 23, for a detection rate of 7.1 per 1,000 screening exams.
There were 107 false positives from both tomosynthesis and ultrasound, for a rate of 3.3% of the total cohort. There was no statistically significant difference between the two modalities in terms of the number of false positives or the number of recalls that led to biopsy, the authors wrote.
Which is better?
Whether a facility would use ultrasound or tomosynthesis as an adjunct to mammography depends on a number of factors, according to Houssami and colleagues. If the final results of the trial confirm the interim data, one could argue that in a setting where ultrasound is commonly used to screen women with dense tissue, tomosynthesis would have little value. But if adjunct ultrasound is not routinely used, tomosynthesis could be a good option -- especially with reconstructed or "synthetic" 2D images, which cut the amount of radiation to which women are exposed.
"If adjunct ultrasound is not routinely performed in mammography-negative dense breasts, then our results could be taken to support use of adjunct tomosynthesis, despite its lower incremental cancer detection rate relative to ultrasound," the group wrote. "The rationale is that through tomosynthesis-based mammography ... a substantial proportion of the additionally detected breast cancers on adjunct ultrasound would be identified through the primary tomosynthesis screen."
But ultrasound's higher cancer detection rate compared to tomosynthesis is hard to dismiss, according to an accompanying editorial written by Dr. Wendie Berg, PhD, of Magee-Womens Hospital in Pittsburgh.
"On the basis of the results from ASTOUND, tomosynthesis still misses a substantial number of invasive cancers in women with dense breasts," she wrote. "Ultrasound ... should be seen as a supplement to mammography where both are available."
More research is needed, Houssami and colleagues conceded.
"Policy on adjunct screening in women with dense breasts should consider whether the screening context routinely provides ultrasound to these women and that tomosynthesis could potentially be the primary imaging modality," they wrote. "This issue requires careful health-economic evaluation to complement the data we have presented."