A deliberate and strategic merger of radiology and pathology into a unified specialty is essential if both disciplines are to survive in the era of AI. That’s the view of two luminaries in a commentary posted on 8 October by the European Journal of Radiology AI.
“Calls for a merger between radiology and pathology are gaining momentum, driven by the rapid evolution of AI and its capacity to unify image-centric disciplines,” wrote Prof. Evis Sala, chair of diagnostic imaging and radiotherapy at Fondazione Policlinico Universitario Agostino Gemelli IRCCS in Rome, Italy, and Prof. Mathias Goyen from the University of Hamburg, Germany, and GE Healthcare. “While some critics argue that AI will simply augment existing workflows, we contend that it will fundamentally reshape them, making the case for a unified specialty both logical and urgent.”
Radiologists and pathologists share a common mission to interpret visual data and extract clinically actionable insights, but they operate in silos, often duplicating efforts and missing opportunities for synergy, the authors explained. “AI disrupts this paradigm by enabling seamless integration of radiological imaging, histopathological analysis, and molecular profiling. The result is a richer, more holistic understanding of disease, one that transcends traditional boundaries.”
The concept of the “diagnostician” -- a physician trained in both imaging and pathology -- is no longer theoretical and is a necessary evolution in response to the demands of precision oncology, adaptive radiotherapy, and personalized medicine, they wrote. “Academic institutions and multinational corporations are already pioneering integrated diagnostic workflows, demonstrating the feasibility and clinical value of this approach.”
They admit that the idea of a merger is an ambitious proposal, but not without its complexities.
“Rather than viewing these challenges as barriers, we propose they be seen as opportunities to improve healthcare delivery and professional practice,” noted Sala and Goyen. “The integration of radiological images, histopathological slides, and molecular profiles presents a formidable challenge. However, it also offers a unique opportunity to develop standardized, interoperable platforms that unify diagnostic data streams. AI-powered tools can harmonize diverse datasets, enabling clinicians to extract richer insights and deliver more precise, patient-centered care.”
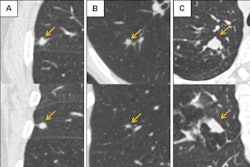
Consider a patient with suspected lung cancer, they explained. “In an integrated diagnostic model, imaging findings (e.g., spiculated nodule morphology) are immediately correlated with histopathological features and molecular markers (e.g., epidermal growth factor receptor [EGFR] status), enabling a unified report that guides targeted therapy. This kind of collaborative workflow, supported by AI, exemplifies the potential of a diagnostician-led approach to streamline decision-making and improve outcomes.”
The future diagnostician will be a hybrid professional equipped to interpret imaging, analyze tissue, understand molecular signatures, and apply AI-driven insights to clinical care, the authors noted. “Achieving this vision, however, demands systemic change, new training programs, redefined roles, and a reimagined healthcare infrastructure.”
Debate on social media
The EJR AI article has already generated a lively debate on social media.
“Given the nuances of the individual specialties, I think combining to one specialty will be challenging,” noted Prof. Nuala Healy, chair of radiology at Dublin’s Beaumont Hospital on LinkedIn. “I think going forward the two specialties, in particular in the field of breast, will become more closely aligned, collaborating with each other and AI to deliver optimal diagnostic reports, prognostication, and prediction.”
According to Dr. Tim Leiner, PhD, professor of radiology at the Mayo Clinic, Rochester, Minnesota, U.S., “This is a logical step in my opinion!”
Acknowledging that AI-driven analysis of imaging connects radiology and pathology is correct, but this is only a fraction of the radiologist’s value, stated Dr. Firdaus Mohamed Hoesein, PhD, a cardiothoracic radiologist at UMC Utrecht in the Netherlands.
“Our core expertise extends beyond pattern recognition to complex clinical consultation, interventional procedure guidance, safety protocols (e.g., contrast), and real-time triage,” he pointed out, also on LinkedIn. “Reducing our specialty to image interpretation -- even AI-enhanced -- is a failure to recognize the holistic, procedural, and immediate diagnostic role we play in patient care. The 'diagnostician' risks becoming AI-dependent and clinically incomplete.”
You can read the full EJR AI article here.