As healthcare systems face rising demand and persistent workforce pressures, the need for streamlined and efficient clinical pathways has never been greater. In medical imaging, AI holds promise not just as a diagnostic tool but as a key enabler of better workflow.
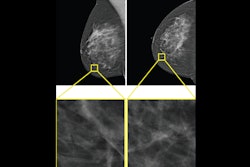
In Signify Research’s 2024 market report on AI in Medical Imaging, a 21% compound annual growth rate (CAGR) was projected for the global market over the report’s forecast period. In our 2025 update, that projection has been revised to 17.7%. While still a strong growth trajectory, the downward adjustment reflects growing recognition that technical performance alone is not sufficient to drive sustainable adoption.
 A graph representing the market size for the total AI in medical imaging market from 2024 to 2029.Signify Research
A graph representing the market size for the total AI in medical imaging market from 2024 to 2029.Signify Research
To date, much of the focus around AI has focused on algorithmic accuracy. However, accuracy alone does not translate to clinical value without seamless integration into the imaging process. The real opportunity lies in how AI supports the broader workflow, accelerating decision-making, reducing bottlenecks, and improving coordination across teams. Hospitals and imaging networks are beginning to shift their expectations. Rather than standalone tools, they are looking for solutions that enhance the entire imaging journey, from referral and triage through to reporting and follow-up. In this context, the future of AI in imaging will not be defined only by the smartest algorithm but also by the smartest integration.
To drive real impact, AI tools must become part of the daily rhythm of care, guiding decisions from referral through image acquisition, interpretation, reporting, and follow-up. This requires integration across the full clinical stack, including PACS, RIS, and electronic medical record systems. Without this interoperability at the workflow level, AI tools remain disconnected from the people and processes that shape patient care. Stroke imaging provides a compelling example of what is possible when this integration is achieved. In these pathways, AI is not just detecting abnormalities, it is triggering alerts, enabling faster team communication, and ultimately supporting time-critical decisions. Cardiology, by contrast, is still in the early stages of this transformation.
Many tools remain focused on discrete tasks, with limited interaction across the broader care process. For vendors, this highlights a critical opportunity. The most successful solutions will be those that support a joined-up pathway, align with how clinicians work, and position themselves as essential workflow enablers rather than optional add-ons. This shift unlocks multiple advantages, including higher adoption, broader clinical relevance, and the potential to scale beyond isolated use cases into enterprise-wide platforms. For providers, it means investing in tools that do more than deliver a result; they support the full journey of care.
Even with growing recognition of the need for workflow integration, many AI tools still struggle in real-world settings. The issue is less about technical performance and more about poor alignment with the clinical environment. Imaging departments face structural barriers, including legacy systems, workforce constraints, and fragmented responsibilities across teams. New tools are often procured without adequate planning for how they will fit into local pathways or how implementation will be supported.
As a result, even strong technologies can fail to deliver meaningful value. Vendors sometimes assume integration will follow once performance is proven, but in practice, adoption depends on early attention to workflow fit, stakeholder engagement, and sustained support. Addressing these challenges is critical to unlocking the broader benefits of AI, from improved consistency and efficiency to better staff experience and patient outcomes. Scalable impact will come from solutions that embed naturally into clinical routines, not from those that remain technically impressive but operationally disconnected.
There are signs that the market is beginning to adjust to these realities. A growing number of vendors are shifting focus from algorithmic performance alone to developing AI solutions that are operationally viable and workflow-conscious. As core tasks like image triage, abnormality detection, and segmentation become widely replicated across tools, the underlying algorithms are beginning to commoditize.
For providers, this evolution is equally important. Procurement decisions are increasingly influenced by how well a solution fits existing pathways, supports pressured teams, and drives operational efficiency. Evaluation criteria now include measurable outcomes such as time savings, reporting consistency, and throughput gains. For vendors, this presents a strategic opportunity. Building workflow-focused layers enables them to move beyond one-off sales and toward long-term service relationships with health systems. It also provides a route to scale across multiple specialties, embedding deeper within IT and operational infrastructure. In this context, AI becomes less a standalone product and more a platform capability, one that supports workforce capacity, improves system resilience, and positions vendors as partners in care delivery rather than tool providers.
Even with better workflow design and stronger alignment between vendors and providers, challenges remain that limit the wider impact of AI in imaging. Many solutions are still confined to narrow use-cases or single departments, struggling to scale across specialties or link meaningfully with broader care processes. In many cases, valuable data remains locked in silos, making it difficult to coordinate care or extract insights across different parts of the patient journey. As the sector matures, the focus will need to shift toward a more connected and integrated workflow, where imaging data, clinical findings, and decision-support tools work together across teams, systems, and settings. Achieving this vision will depend on developing tools that can operate within more open and responsive environments, where information flows reliably and clinical context is preserved across each step of the pathway.
Emerging data standards and platform strategies are beginning to support this evolution, offering new ways for AI to support not just local efficiency but system-wide coordination. However, these advances will only create value if the foundational work of embedding AI into real clinical workflows is already in place. A more integrated future is possible, but only if vendors first succeed in building tools that are usable, adoptable, and genuinely embedded at the front line of care.
The future of AI in medical imaging will not be shaped by the most advanced algorithms but by the most effective implementations. Embedding AI into workflow is not a technical afterthought; it is the defining factor that determines whether a tool delivers real value or fades into irrelevance. For providers, this means shifting evaluation criteria to focus on operational impact and service alignment. For vendors, it requires a commitment to designing for real clinical environments, supporting adoption, and addressing the day-to-day pressures faced by imaging teams.
When AI becomes an enabler of care rather than a separate layer, it can play a powerful role in reducing backlogs, improving reporting consistency, and relieving pressure on stretched workforces. The opportunity is not simply to automate tasks but to build a more connected, responsive, and resilient imaging service. That future is within reach, but only if workflow remains the starting point, not the end stage, of AI innovation.
 Umar Ahmed from Signify Research.
Umar Ahmed from Signify Research.
Umar Ahmed is a market analyst with Signify Research’s AI healthcare team.
The opinions expressed in this review are those of the author and do not necessarily reflect the views of AuntMinnieEurope.com.