VALENCIA - As the global shortage of radiology specialists increases, only adopting "the 7P approach" (practicality, pragmatism, product, price, place, promotion, and passion) to the implementation of artificial intelligence (AI) can provide the highest levels of safety with fewer resources. That's the view of AI guru Dr. Sergey Morozov.
"It's a step that you take and build on. Hospitals want to invest in AI to save money and improve health outcomes," he said on 15 October at the annual congress of the European Society of Medical Imaging Informatics (EuSoMII).
Practicality should prevail when choosing a new solution. "We should be facing the truth and not expect AI to be a magic," said Morozov, who is chief innovation officer at the Belgian software developer Osimis, EuSoMII past president, and the former chief regional radiology officer for Moscow.
 Cloud-based AI algorithms are the most promising, Morozov says.
Cloud-based AI algorithms are the most promising, Morozov says.AI is classified as "Software as a Medical Device (SaMD)" for automation of radiologists' work. Most systems file under Class IIA category, as Class IIB would make them autonomous devices, therefore more expensive because liable.
"Liability requires insurance, which means the price is two to three times higher than a non-autonomous device," he said. "The hospital that buys an autonomous device must reduce the workforce otherwise they would be spending money in vain."
An AI product should be fully automated and not simply available on-demand, according to Morozov.
Demonstrating accuracy and economic efficiency
When looking at performance metrics, sensitivity should be 97% or higher in order not to miss pathology, and specificity should be at least 85%.
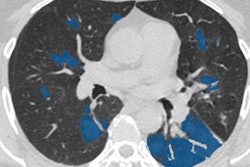
False negatives can be minimized by fine-tuning a threshold during the deployment phase, in order not to miss a single case. One should watch out then for false positives, Morozov advised. "We used to think this was not a problem, but we should be aware of typical cases. Otherwise, there may be over-reliance from radiology trainees, who still need to learn to read images alone."
False positives may also trigger more work, he added. "Some hospitals started to include AI references in their reports, indicating when it was wrong. Having to explain that to patients, that just creates more work."
Although specificity is not the focus, it should be augmented, according to Morozov.
Current AI products are perfectly accepted by radiologists and other referring physicians, he believes. "They enjoy having AI in the hospital because it creates a higher level of trust from patients, who see that the hospital is so mature that it can provide beautiful AI-powered protocols."
Being able to demonstrate return on investment (ROI) is essential and should be scaled into four different phases, building from protection against a missed pathology, to increased productivity, workload redistribution, providing results directly to a referring physician, and managing the demand for the radiology workforce.
"For example, many hospitals in France only have one radiologist in the emergency department once or twice a week. So they have no other choice but to do reporting and make use of images taken by the emergency physicians on their own," noted Morozov.
There are several studies that demonstrate economic efficiency brought by AI, whether for quality improvement, saving time, improving the workload, or automating the workflow.
"Perspectives are very good," he said.
Place and promotion
Radiologists should decide where they wish to buy an AI product from: the market or as part of a platform.
"The market is a fancy place to try out things here and there, but the platform approach or direct integration makes more sense, because it's more about the volumes, and a rational choice for the long-term contract," he said.
He also noted that there is a clear tendency to shift from on-premises to cloud-based AI because it "brings the beauty of freedom and ease of integration."
Algorithms that are cloud-based are the most promising and there shouldn't be too many interfaces. "Less is more."
As for economics' behavior, the choice is not always rational. "Typically, one studies the pros and cons, and eventually purchases the red Ferrari car," Morozov said.
With AI, many hospitals want to show that they are mature and strong. Innovators often tend to make an emotional or behavioral choice, but there should be people who do rational buying in the team. Promotion often comes from the early adopters themselves.
Every AI tool should present like a tablet and clearly state its indications and contraindications. "There should be sensitivity and specificity, and potential false positives -- 'contraindications' -- for the physician or patient's notice," Morozov said. "That's probably the way to improve transparency rather than trying to build transparency by playing somewhere in the background with neural networks."
In the end, AI must be integrated directly in the reporting (RIS and PACS) workflow in such a way that it does not add extra burden to radiologists, he insisted. "The workflow must be robust enough to ensure AI analysis is complete and available on PACS, before a specialist starts image interpretation," he concluded.