Radiologists reporting prostate multiparametric MRI (mpMRI) exams must be familiar with the latest recommendations of Prostate Imaging Reporting & Data System (PI-RADS v2.1) and the potential pitfalls mimicking malignant lesions during diagnosis, active surveillance, and recurrence assessment, a leading Spanish research team has asserted.
"Normal anatomic structures and benign conditions can mimic prostate cancer on mpMRI. Knowledge of the common pitfalls is essential for radiologists who interpret mpMRI," noted Dr. Daniel Vas and colleagues from Hospital Clínic de Barcelona in an e-poster that won a cum laude award at ECR 2023.
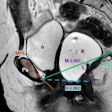
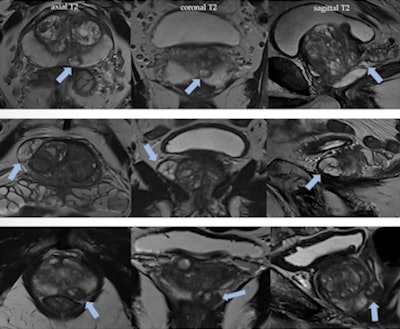 Benign prostatic hyperplasia nodules in the peripheral zone may mimic prostate cancer. Nodules with typically glandular type hyperplasia may appear in peripheral zone as ectopic or herniated nodules from the transition zone. It is important to analyze the morphology on T2-weighted imaging; look out for well-defined, rounded, encapsulated lesions; and identify the hyperintense component corresponding to hyperplastic glands with cystic ectasia. Figures courtesy of Dr. Daniel Vas et al and presented at ECR 2023.
Benign prostatic hyperplasia nodules in the peripheral zone may mimic prostate cancer. Nodules with typically glandular type hyperplasia may appear in peripheral zone as ectopic or herniated nodules from the transition zone. It is important to analyze the morphology on T2-weighted imaging; look out for well-defined, rounded, encapsulated lesions; and identify the hyperintense component corresponding to hyperplastic glands with cystic ectasia. Figures courtesy of Dr. Daniel Vas et al and presented at ECR 2023.Also vital is a sound knowledge of the basic concepts of the Prostate MRI for Local Recurrence Reporting (PI-RR) after radiation therapy and radical prostatectomy and the Prostate Cancer Radiological Estimation of Change in Sequential Evaluation (PRECISE) scoring system in men on active surveillance for prostate cancer, they reported.
Provide the key points that should appear in the radiological report -- applying PI-RADS, PI-RR, and PRECISE criteria -- that are essential to patient management, the authors added.
"PI-RADS is designed to standardize image acquisition techniques and interpretation of prostate MRI for the detection of clinically significant prostate cancer," they explained. "By periodic updates, modifications are made with the purpose of improving interreader variability and simplifying PI-RADS assessment. PI-RADS v2.1 adopts a series of recommendations in order to improve even more the diagnostic performance of mpMRI."
The purpose of PI-RR is to standardize the evaluation of local recurrence of prostate cancer using MRI after radiation therapy and radical prostatectomy, while PRECISE gives recommendations for reporting of MRI studies in men on active surveillance for prostate cancer.
Clinical issues
In particular, mpMRI is recommended over biparametric MRI (bpMRI) when the clinical context and risk factors indicate the presence of probable significant disease that should be screened for (e.g., family history, previous negative biopsy with elevated PSA, patient on active surveillance), according to the authors.
Other situations in which to prefer mpMRI are when a previous negative bpMRI result gives rise to persistent suspicion or when technical factors possibly condition suboptimal diffusion-weighted imaging (DWI) quality, as in the case of a hip implant.
The reasearchers think the main clinical considerations are as follows:
- Antispasmodic agents may be beneficial
- No consensus on microenema prior to MRI (may promote peristalsis)
- Evacuate rectum before study
- There is no clear evidence that abstention from ejaculation 72 hours prior to MRI alters the result
- Postbiopsy hemorrhage is not likely to compromise the diagnosis of clinically significant cancer, as postbiopsy changes may persist, an interval of at least six weeks between the biopsy and MRI is still should be considered.
Also, they listed the key points to include in the radiological report as prostate volume (up to four lesions gives PIRADS > 2); the dominant lesion (locate according to the prostate sector map); lesion measurements (on apparent diffusion coefficient [ADC] in peripheral zone, T2 in tertiary zone); signs of extraprostatic extension, lymph node or pelvic bone involvement, and other detected findings (urinary bladder, ureters, colon, etc).
Pitfalls to keep in mind
Acute and chronic prostatitis can cause signal changes in both the peripheral and transition zones that are indistinguishable from prostate cancer, and they should be evaluated by applying the PI-RADS v2.1 system, assigning the corresponding category, the authors wrote.
An evolved acute prostatitis may present with intraglandular abscess formation as a complication with the following MRI characteristics: hyperintense on T2-weighted imaging, ring enhancement, restricted DWI, and diffusion on ADC.
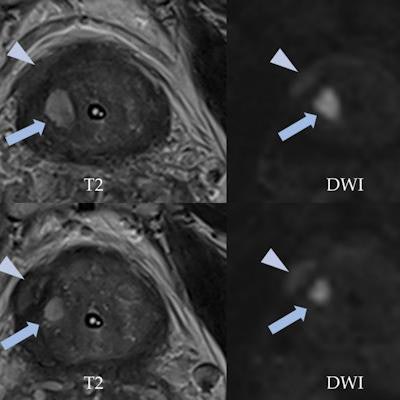
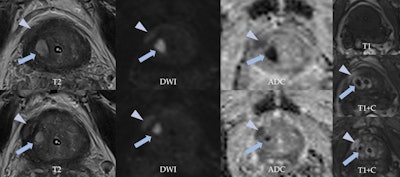 A 69-year-old man with urinary retention and recurrent prostatitis with chronic urinary catheter had a PSA of 3.79 ng/ml. MpMRI shows round, high signal intensity lesion on T2-weighted imaging in the right transitional zone (arrows), highlighting markedly restricted diffusion and "ring" peripheral contrast uptake, consistent with a small abscess. A lenticular area is visualized in the right peripheral zone (arrowheads), showing characteristics of a PI-RADS 4 lesion (restricted diffusion and low T2 signal intensity, contrast uptake). However, malignancy was suspected due to mpMRI, and taking into account the accompanying findings, it was thought this might correspond to a phlegmonous area (prostatitis).
A 69-year-old man with urinary retention and recurrent prostatitis with chronic urinary catheter had a PSA of 3.79 ng/ml. MpMRI shows round, high signal intensity lesion on T2-weighted imaging in the right transitional zone (arrows), highlighting markedly restricted diffusion and "ring" peripheral contrast uptake, consistent with a small abscess. A lenticular area is visualized in the right peripheral zone (arrowheads), showing characteristics of a PI-RADS 4 lesion (restricted diffusion and low T2 signal intensity, contrast uptake). However, malignancy was suspected due to mpMRI, and taking into account the accompanying findings, it was thought this might correspond to a phlegmonous area (prostatitis).With larger collections, transrectal drainage can be useful to help resolution and patient recovery. "It is recommended to carry out follow-up MRI of a suspicious lesion detected during acute prostatitis with abscesses if it is not examined by biopsy," they noted.
In cases of granulomatous prostatitis, uncommon chronic inflammation is usually detected by histopathological analysis of a biopsy, since the MRI appearance can be identical to a suspicious PI-RADS 4/5 lesion. Idiopathic etiology exists in about 60% of patients and may be associated with previous treatment of bladder cancer with Bacillus Calmette-Guerin, a type of immunotherapy drug.
Evolving process
An important aspect to bear in mind is that the initial PIRADS consensus defines the document as a "living" report that will evolve based on clinical experience and data acquisition, and the same can be said about PRECISE and PI-RR, Vas told AuntMinnieEurope.com.
There are numerous ongoing studies and recent papers regarding the application of biparametric MRI, the usefulness of contrast media to differentiate PIRADS 3 from true PIRADS 4 lesions, and the inconclusive need for gadolinium in patients on active surveillance, which are the main fields of interest, he remarked.
The co-authors of the ECR e-poster were Rafael Salvador, Daniel Corominas Muñoz, Laura Buñesch, Carmen Sebastià Cerqueda, and Carlos Nicolau.