Many patients -- and even radiologists' clinical colleagues -- have unrealistic expectations of what medical imaging can deliver, said Dr. Giles Maskell in a keynote lecture at the British Institute of Radiology (BIR) Annual Congress on 23 September.
 Dr. Giles Maskell.
Dr. Giles Maskell."There seems to be a general expectation that reading an x-ray is like reading a newspaper: The answer just comes out and it should be right every time. Whereas people who do the job, the radiologists, know that it's a process of interpretation and sometimes it's actually quite difficult to decide one way or another what the answer is," noted Maskell, who is a consultant radiologist at Royal Cornwall Hospitals NHS Trust and past president of the U.K. Royal College of Radiologists.
Some abnormalities can be very subtle to discern and sometimes "for all sorts of perceptual and cognitive reasons, we just don't see things that are there in front of us," he added. "But we haven't really got that message across to the public as a whole -- the fact that someone said your x-ray is clear isn't always a complete guarantee that it is."
Maskell said that a radiologist's role is constantly evolving. Many of the typical daily tasks done by a junior radiologist in 1985 were now either obsolete -- such as barium meals, venograms, lymphangiography -- or mostly performed by other people, such as gallbladder and renal tract ultrasound. This means radiologists' beliefs and assumptions had to be frequently reassessed.
"What is accepted as the truth today may not be the truth in 10 to 20 years' time," he said.
Often people expect radiology to deliver the correct answer "every time," according to Maskell. "We know that this is not deliverable. Sooner or later we are going to have to address this knowledge gap."
It is the duty of radiological societies and leadership bodies to do more to educate people about the limitations of imaging tests and how they are interpreted.
Relationships with patients
Over time, radiologists have allowed the link between themselves and the patients to become thinner and thinner, while keeping a strong bond with the clinician, he continued.
"There are notable exceptions to this, such as breast and interventional radiologists, but most of us have allowed that link to be very tenuous and have almost hidden behind the clinician, and I don't think it's to our benefit or the patient's benefit," Maskell told BIR delegates.
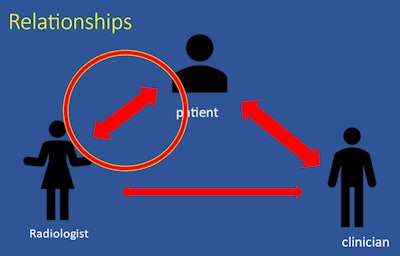 Radiologists must strengthen their relationships with patients, according to Maskell.
Radiologists must strengthen their relationships with patients, according to Maskell.He noted how demand for imaging kept rising -- driven partly by changes in clinical practice, such as cancer therapeutics, system developments including remote consultations, other "scan first" practices and "pressures" in emergency departments, and the change in society's approach to risk. There was now more "defensive medicine" arising from less tolerance of uncertainty and radiologists weren't immune to this, he said.
Radiologists themselves are "contributing to the problem" through the pursuit of incidental findings, and higher resolution images are resulting in more findings of uncertain significance, Maskell explained.
"The harder we look, the more we find. Poor quality clinical information compounds the problem -- if there is no clear clinical question, there are no incidental findings." he said
Furthermore, the practice of dismissing incidental findings is becoming harder and harder to justify, particularly for those working for an outsourcing or teleradiology company, where the radiologists' work is being audited and where they know they will be picked up on for every little thing they don't mention, he noted.
"30 years ago, we had a pretty clear idea of what was an appropriate use of imaging and what was inappropriate, now it's not quite so clear," he said.
Maskell said radiologists needed to reexamine "what we do, for whom, how much good it does, what the value is in it and generally making a balanced decision on that."
"Are we moving towards a point, with CT in particular, where the detection of clinically unsuspected abnormalities becomes the main purpose of the study, and what does that mean for the concept of appropriateness?" he asked attendees.
On a positive note, he also said radiology had moved on from being perceived as a solitary profession to one where the vital importance of teamwork and learning from feedback to help improve performance was more recognized.