Awareness, imaging delay, and choice of protocol are key to differentiating between pulmonary fibrosis and the "fibrotic-like" changes of COVID-19 that mimic it. During the "Thoracic manifestations of COVID-19 pneumonia in 2022: New insights" session at ECR Overture on 4 March, listeners had the chance to discover the longer-term radiological appearances of the disease and why the correct choice of terminology is crucial to follow-up.
Dr. Katharina Martini, consultant chest radiologist at Zurich University Hospital noted that in the literature, 94% of patients show residual findings at discharge -- although this number might be artificially high, as not all patients undergo CT at discharge.
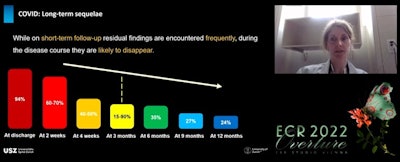
"While in short term follow-up residual findings are encountered frequently, during disease course they are likely to disappear," Martini noted. "However, we're not yet sure how many patients will develop persistent pulmonary changes after COVID-19."
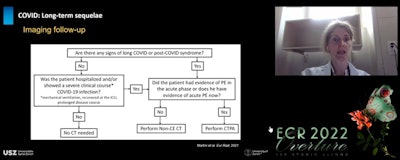
Discussing the long-term sequela of COVID-19, she noted that follow-up imaging should be performed after a delay to allow for resolution of the reversible inflammatory process, and she pointed to recommendations for CT follow-up at 12 weeks post discharge in patients with persistent respiratory symptoms after clinical assessment and pulmonary function test evaluation. She also referred to the European Society of Thoracic Imaging's flowchart on how and when to image COVID-19 patients.
The appearance of acute stage COVID-19, with peripheral and bilateral ground-glass opacities (GGO), followed by consolidation and then resolution in survivors is well-documented. However, at discharge, GGO may extend further into the lung while decreasing in attenuation. This is known as the "tinted sign," possibly reflecting a regression of inflammation and associated with reexpansion of the alveoli.
"This should not be mistaken for progression of disease," noted Martini.
Erroneous terminology
Remaining CT abnormalities are reported in 15% to 90% of COVID pneumonia patients at three months post discharge, the higher range being reported in patients previously admitted to the intensive care unit. But it is expected that these signs will reverse in the vast majority of cases. Besides largely resolved low attenuation GGO, in these patients, follow-up imaging might show other fibrotic-like findings such as linear consolidation, parenchymal bands, and perilobular opacities consistent with organizing pneumonia as well as reticulation, interstitial thickening, and bronchial distortion.
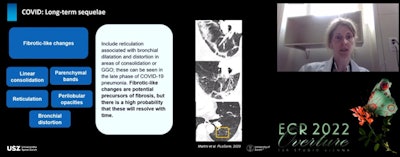
At three months post discharge, fibrotic-like changes, seen in the late stage of COVID-19 pneumonia, are reported in 21% to 26% of patients. In these cases, it is important to word findings carefully, and the difference between fibrosis and what is "fibrotic-like" must be clear for fear of overestimating them, Martini told listeners, While the latter can be precursors to fibrosis, there is a high probability these changes will resolve with time.
"The term traction bronchiectasis, suggesting irreversible fibrotic changes, should be used with caution. It's better to use the term bronchial distortion or bronchial dilatation," Martini noted. "Honeycombing is also an uncommon finding in COVID-19. If we see it, it is more likely that the patient has a pre-existing fibrotic lung disease than it being due to COVID."
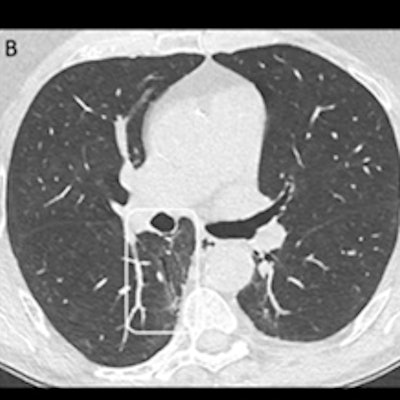
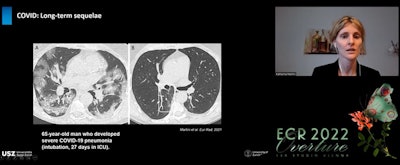 (A) CT shows a 65-year-old patient in subacute stage with bilateral ground-glass opacities and consolidation and in posterior lung area, signs resembling COP. (B) After six months, consolidation has mainly resolved but some ground-glass opacities remain in posterior right zone of lung and within this, an area of bronchial distortion.
(A) CT shows a 65-year-old patient in subacute stage with bilateral ground-glass opacities and consolidation and in posterior lung area, signs resembling COP. (B) After six months, consolidation has mainly resolved but some ground-glass opacities remain in posterior right zone of lung and within this, an area of bronchial distortion.Another interesting three-month finding on CT is mosaic attenuation pattern with areas of hypoattenuation in patients who had severe or critical disease, noted Martini. This mosaic attenuation can be best visualized in minimum intensity projection (MIP) and might be due to either microvascular obstruction or residual small airway disease.
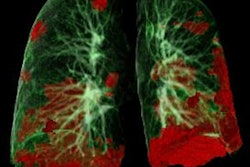
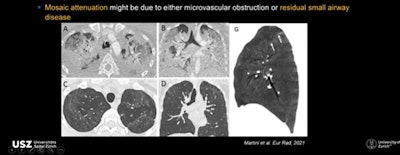 CTs show mosaic attenuation pattern due to microvascular obstruction or residual small airway disease.
CTs show mosaic attenuation pattern due to microvascular obstruction or residual small airway disease.At 12-month follow-up, most changes have resolved with only 24% of patients showing abnormal CT findings, and the spectrum of these findings also changing, noted Martini. Typical fibrotic-like features such as interlobular septal thickening and reticular opacity almost disappear by month nine to leave only GGO as the predominant residual finding. Established fibrosis or interstitial thickening is not observed.
Discussion topics
But from which time point will visualized lung changes be permanent? This was a question from moderator Dr. Jürgen Biederer, head of imaging and section chief of pulmonary imaging in the department of diagnostic and interventional radiology at University Hospital Heidelberg, Germany.
 Dr. Jürgen Biederer.
Dr. Jürgen Biederer.Martini stressed that it was difficult to call because of the lack of long-term follow-up studies.
According to Dr. Marie-Pierre Revel, PhD, head of cardiothoracic imaging at Hôpital Cochin in Paris, anomalies seen at one year post discharge are unlikely to resolve.
"At six months post discharge it is likely that we can predict that at one year the patient will still have anomalies," she noted.
Revel, who presented, "What's the current role of imaging?" during the session pointed to mosaic attenuation as the most intriguing of the signs with its potential cause of small airway disease or vascular occlusion.
 Dr. Marie-Pierre Revel, PhD.
Dr. Marie-Pierre Revel, PhD."I've noticed only the severe cases have the most abnormal total lung capacity (TLC) changes. I would suspect a vascular phenomenon rather than fibrotic changes -- which would affect the volumes. Only the diffusion capacity is abnormal," Revel noted.
And what about patient position -- should they be imaged prone or in supine position and would the experts add in expiratory scans? Martini noted that most patients are scanned in supine position.
"Expiratory scanning can be helpful to capture some alterations, but I wouldn't do it on a regular basis, especially if the patient is young," she said.
The panel also responded to a question about CT's return to its prepandemic role.
Biederer noted that in an environment with a high prevalence of COVID-19, CT has a high predictive value, but this dilutes when other diseases are also prevalent. Martini concurred adding that with other viral infections such as influenza which has similar CT alterations, once the pandemic is over CT loses its specificity for COVID-19 detection.
"But the pandemic isn't over," noted Revel. "The best combination is RT-PCR tests and CT because in patients with dyspnea and low saturation it has a major prognostic role. The combination is really important in patients with respiratory distress or in fragile patients as they need to be treated and avoid long-term sequelae."