The growth of prostate MRI has led to an increase in the number of incidental findings, some of which may be clinically significant, and radiologists should play a central role in their detection, according to Spanish researchers.
"Prostate MRI is the best imaging modality for the diagnosis, staging, and evaluation of the response in prostate cancer," noted Dr. Eduardo Alvarez-Hornia Pérez, a radiologist at Clinica IMQ Zorrotzaurre in Bilbao. "In the evaluation of prostate MRI, it is also possible to detect incidental findings included in the field of study. Many of these incidental findings are benign, but some of them could have clinical implications."
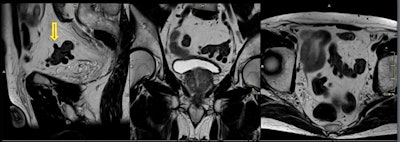
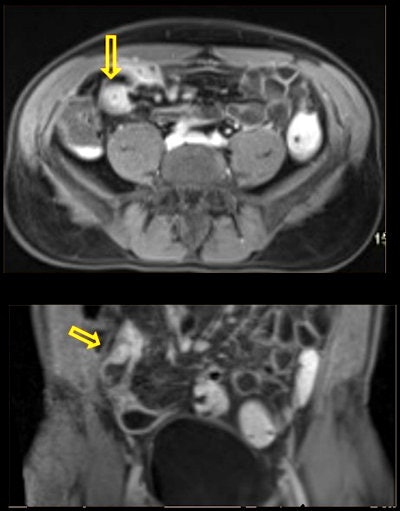 58-year-old man with a history of diffuse abdominal pain. Incidental finding on prostate screening: ileal wall thickening and increased mural contrast enhancement, suspicious of intestinal inflammatory disease. Crohn's disease was confirmed posteriorly. All figures courtesy of Dr. Eduardo Alvarez-Hornia Pérez.
58-year-old man with a history of diffuse abdominal pain. Incidental finding on prostate screening: ileal wall thickening and increased mural contrast enhancement, suspicious of intestinal inflammatory disease. Crohn's disease was confirmed posteriorly. All figures courtesy of Dr. Eduardo Alvarez-Hornia Pérez.It is important that radiologists look beyond the prostate and accurately recognize and characterize incidental findings, differentiating indolent entities from clinically significant pathologies and avoiding error in diagnosis and treatment, Alvarez-Hornia and colleagues noted in an e-poster presented at ECR 2021.
They performed a retrospective review of the 679 prostatic MRI performed in their facility during 2019, assessing the incidental findings described in these studies. Their aim was to illustrate the extraprostatic findings present in these patients.
Genitourinary incidental findings
In their analysis, they identified the following genitourinary incidental findings:
- Utricular cysts: midline area of focal dilatation that occurs within the prostatic utricle
- Cowper's gland duct cyst: midline oval structure at the penile base adjacent to the ventral aspect of the proximal bulbous urethra
- Seminal vesicle hemorrhage: hyperintense signal at precontrast T1-weighted MRI is indicative of hemorrhage in the seminal vesicles as well as in the prostate
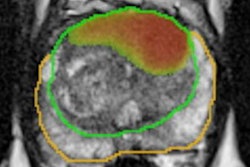
 67-year-old man with vesicle cancer. High prostate-specific antigen (PSA) level and hematuria. Incidental finding: polypoid lesion on anterior wall of bladder with restricted diffusion and contrast enhancement.
67-year-old man with vesicle cancer. High prostate-specific antigen (PSA) level and hematuria. Incidental finding: polypoid lesion on anterior wall of bladder with restricted diffusion and contrast enhancement.- Hydrocele: acquired or congenital serous fluid collections between the layers of the tunica vaginalis surrounding a testis or spermatic cord
- Bladder hernia: herniation of the urinary bladder is a relatively uncommon condition that occurs when the urinary bladder herniates into the inguinal canal
- Bladder diverticulum: herniation of bladder mucosa between fibers of the detrusor muscle
- Bladder stones: hardened clumps of minerals that form in the bladder
- Diffuse thickening of the bladder wall: "If the bladder wall is adequately distended, then a differential may be developed based on whether the bladder is diffusely thickened or focally thickened: bladder outlet obstruction, neurogenic bladder, infectious cystitis, cystitis from radiation or chemotherapy," the authors stated.
- Bladder neoplasm: focal bladder wall thickening due to a primary neoplasm of the urinary bladder
Nongenitourinary incidental findings
They also encountered the following nongenitourinary incidental findings:
- Inguinal hernia: An inguinal hernia occurs when the intestines or fat from the abdomen bulge through the lower abdominal wall into the inguinal, or groin, area.
- Diverticular disease: Diverticulosis is the condition of having multiple pouches (diverticula) in the colon that are not inflamed. These are outpockets of the colonic mucosa and submucosa through weaknesses of muscle layers in the colon.
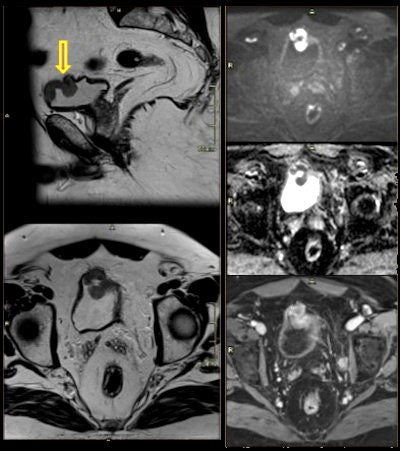
 74-year-old man with diverticular disease. Incidental finding on prostate screening: multiple diverticula of the sigmoid colon without evidence of diverticulitis.
74-year-old man with diverticular disease. Incidental finding on prostate screening: multiple diverticula of the sigmoid colon without evidence of diverticulitis.- Inflammatory bowel disease: This term is used for two conditions (Crohn's disease and ulcerative colitis) that are characterized by chronic inflammation of the gastrointestinal (GI) tract. Prolonged inflammation results in chronic damage to the GI tract.
- Rectal lesions: focal wall thickening due to primary neoplasms or metastasic disease
- Rectal or perianal fistula: narrow cavity or channel stretching between the bowel and the skin
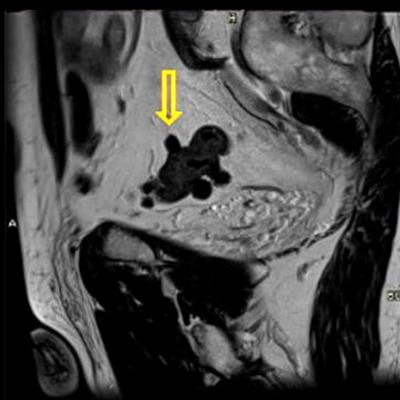
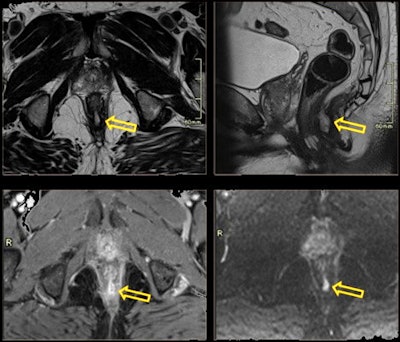 68-year-old man with rectal fistula presented for prostate screening and complained of rectal discomfort. Posterior fistula and abscess were discovered.
68-year-old man with rectal fistula presented for prostate screening and complained of rectal discomfort. Posterior fistula and abscess were discovered.- Presacral fibrosis: Presacral soft tissue is found in up to half of patients after treatment for rectal cancer.
- Lymphangioma: presacral cystic lesions
- Bone lesions, fractures, bursitis, degenerative osteoarthritis of the hip, and metastatic or primary bone lesions
Overall, the authors emphasize the importance of a complete evaluation of the radiological studies to avoid diagnostic errors. Errors of omission are not uncommon in radiological practice and are avoidable, they commented.
Double-reading protocol
The Bilbao group has also found that a double-reading system is a valuable tool to minimize errors in the evaluation of prostatic MRI.
"It favors a homogeneous, uniform, and comprehensible reporting style and encourages communication between the radiologists themselves and with the requesting doctors and increases their confidence in our reports," Alvarez-Hornia and colleagues noted.
They reviewed 396 prostate MRI reports assessed by double reading from January to June 2018. All studies were performed on a 1.5-tesla scanner (Magnetom Avanto, Siemens Healthineers) using a surface coil and following prostate MRI protocol that included T2 turbo spin-echo axial, sagittal, and coronal. All the reports were made and reviewed by four experienced radiologists, each of whom had more than five years of experience in MRI and had reported more than 200 prostate MRI exams.
Of these reports, 97.2% (385 exams) were approved without changes, and there was total agreement in 380 cases (96%). Only 11 cases with discrepancies (2.8% of the reports) required reevaluation and discussion, and only 1.8% involved discrepancy with clinical repercussions. The authors found no statistically significant differences between the radiologists, neither when they acted as first reader nor reviewer.
Editor's note: An open-access article on this topic was posted by Insights into Imaging on 18 March.