Instead of overdiagnosis, the main problem with breast cancer screening is underdiagnosis, according to breast imaging expert Dr. Christiane Kuhl. Furthermore, breast MRI could be a tool of the future to alleviate this problem, she added.
 Dr. Christiane Kuhl from the University of Aachen in Germany.
Dr. Christiane Kuhl from the University of Aachen in Germany.In the run up to the British Institute of Radiology (BIR) annual congress in November, the BIR interviewed several experts, including Kuhl, who is the clinical director for diagnostic and interventional radiology at Aachen University Hospital in Germany. BIR Content Development Editor Miranda Wilson-Wood spoke with Kuhl in a podcast posted on 29 September.
"I certainly think overdiagnosis is not our main problem right now. I think if you ask women for their opinion, most of them would agree -- our problem is still the fact that breast cancer continues to represent the first- or second-most important cause of cancer death in women, and we should try to do something about this," Kuhl said during the interview.
The trouble with overdiagnosis
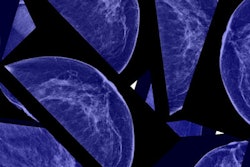
Overdiagnosis is a consequence of using screening mammography -- it detects cancer that if left unchecked would not become lethal. Most estimates of overdiagnosis put the rate from 10% to 30%.
"I don't believe that 30% I have to admit, but 10% maybe, that estimate might be true, and these 10%, most of them, most of the diseases that likely cause such an overdiagnosis are low-grade DCIS [ductal carcinoma in situ]," she said.
Radiologists spot DCIS because it calcifies, and DCIS will never progress into something serious for some patients, but for others it might.
"So what the conclusion we draw right now in the field of breast imaging, also the psychology, is that we try to tailor treatment to the biologic profile of the cancer that's being diagnosed, and a lot of effort goes into trying to better understand the future behavior of a given breast cancer," she said. "This is being done by molecular profile studies but also modern imaging methods. The aim is to administer as much treatment as is necessary to avoid progression to a lethal disease, but also keep your feet still in the case of women's whose cancers are relatively benign and would not progress."
Again though, underdiagnosis is an issue Kuhl is more concerned about. Even with quality assurance in mammography screening programs, the interval cancer rate is between 30% and 50%, which means that one-third to one-half of diagnosed breast cancers are picked up not during screening rounds but in interval rounds. Furthermore, these cancers are associated with a worse prognosis.
"The interval cancer rate is a metric for the success of any given screening program, and with an interval cancer rate of 30% to 50%, we cannot be satisfied, which is the reason why today we strive to improve breast cancer screening methods by, for example, ultrasound, but [also breast MRI]," she said.
The pros of other modalities
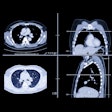
Kuhl is well-known for championing breast MRI. Most recently in February, she and her colleagues published a study about how breast MRI benefits women across all risk categories -- not just those at high risk. In 2016, she discussed the benefits of using an abbreviated breast MRI protocol that could make breast MRI more enticing for widespread use.
"If this concept is reproduced in other trials, and maybe vendors are to manufacture dedicated breast MRI systems as they do with dedicated mammography units, then it is at least conceivable to use breast MRI on a broader scale also for screening," she said.
Breast MRI addresses both over- and underdiagnosis because the modality's high sensitivity means it detects rapidly growing tumors with strong angiogenic and protease activity. However, cost is a major factor keeping MRI from more extensive use, limiting its availability.
"More recent trials, and ... our own experience with MRI, confirm that actually if equivalent expertise is used in the interpretation of an MRI as a mammogram, then the two methods yield about the same specificity and positive predictive value," she said.
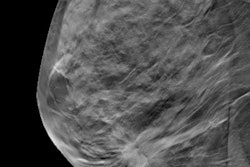
While Kuhl is a fan of breast MRI, she also points out the advantages of other breast imaging techniques such as ultrasound and digital breast tomosynthesis (DBT). Both modalities improve breast cancer detection by highlighting tumors hidden by fibroglandular tissue on regular 2D mammograms. DBT, in particular, is useful in women with heterogeneously dense breasts.
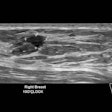
Ultrasound does something similar, but a broad overlap exists between how benign and malignant tissues present, thus leading to a high false-positive rate.
In the future, Kuhl thinks the basis of breast cancer screening will be DBT with synthetic 2D mammograms, (i.e., 2D images acquired from DBT slices). Ultrasound and breast MRI also will continue to have a place in breast cancer screening, she said.
To listen to the full interview, visit the BIR website.