Pulmonary MRI can be used to evaluate acute pulmonary embolism (PE), offering an alternative for patients who can't undergo CT pulmonary angiography (CTPA) or are allergic to iodinated contrast agents, according to Turkish research presented at last week's American Roentgen Ray Society (ARRS) annual meeting.
In a study of 48 patients, Dr. Nevzat Karabulut, of the Pamukkale University School of Medicine in Denizli, Turkey, and colleagues found that three pulmonary MRI techniques yielded performance that could be valuable in a number of clinical scenarios.
Estimates of the annual incidence of PE in the U.S. range from 300,000 to 600,000 (1 to 2 per 1,000), and 10% to 30% of people will die within one month of diagnosis, said Karabulut, who presented the research. MDCT angiography is commonly used to diagnose PE, but not all patients can tolerate CT.
"Multidetector-row CT angiography tends to have high accuracy, but it involves radiation, whereas MRI has no radiation and, if necessary, can be done without gadolinium as well," he said.
The researchers evaluated MR's performance for detecting PE using three techniques:
- Unenhanced balanced steady-state free precession (SSFP) using peripheral gating
- Bolus-triggered breath-hold contrast-enhanced pulmonary MR angiography (MRA)
- Contrast-enhanced recirculation-phase breath-hold low-flip angle 3D gradient echo (GRE)
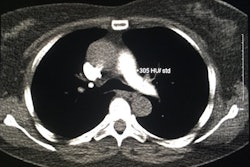
The study included 48 patients with suspected PE who had CTPA first and then an MR exam within 72 hours. Karabulut's group calculated sensitivity and specificity for PE detection for each MR technique, using CTPA as the reference standard. Sensitivity rates for CTPA range from 53% to 100%, while specificity ranges from 83% to 100%, he said.
In the study, CTPA found 340 emboli in 33 of the 48 patients. Sensitivity for PE detection for the three MR techniques was 52% for triggered SSFP, 46% for MRA, and 65% for 3D GRE MRI. MR sensitivity was highest in the right lower lobe (95% for SSFP, 86% for MRA, and 89% for 3D GRE) and lowest in the right middle lobe (29% for SSFP, 50% for MRA, and 83% for 3D GRE) and lingular branch (77% for SSFP, 58% for MRA, and 69% for 3D GRE). Specificity was 98% for triggered SSFP and 99% for 3D GRE MR imaging.
The different MR techniques serve different clinical scenarios and departments, Karabulut concluded.
"Unenhanced SSFP can be used to detect PE at main and lobar pulmonary arteries because it does not require contrast," he said. "And the better performance of the recirculation-phase 3D GRE MR imaging method compared to accurately timed arterial phase MRA could be helpful in emergency settings."
In a related presentation given during the same session, Dr. Seth Kligerman from the University of Maryland explored whether a model-based reconstruction technique could improve the detection of PE compared to both iterative and filtered back projection reconstructions in patients undergoing CTPA.
For their study, Kligerman and colleagues included 25 obese patients (average body mass index, 37.9) and 25 nonobese patients (average body mass index, 24.8) who had undergone CTPA exams. Twenty-two of the 50 patients tested positive for PE. The 50 studies were processed with filtered back projection, iterative reconstruction (iDoseL3, Philips Healthcare), and model-based reconstruction (Philips IMR), for a total of 150 reconstructions.
The images were randomized, and four thoracic radiologists graded each image on a scale of 1 to 5 (with 1 being poor and 5 being ideal) in the following categories: diagnostic confidence, noise, and pulmonary artery enhancement. The readers also marked each study for the presence or absence of PE.
For all four readers, model-based reconstruction showed improved diagnostic confidence, subjective image noise, and subjective pulmonary artery enhancement compared to both filtered back projection and iterative reconstruction in all 50 patients and the subgroup of 25 obese patients, according to the researchers.
In addition, in the 88 studies with PE (22 studies read by four radiologists), the condition was correctly identified in 73 studies using model-based reconstruction, compared with 69 studies using iterative reconstruction and 64 studies with filtered back projection; this was true in both obese and nonobese patients, Kligerman said.