Urgent imaging is increasingly requested by urologic surgeons when postoperative complications are suspected after a prostatectomy, and correct multidetector CT (MDCT) techniques are particularly effective for identifying hematomas, active bleeding, and extravasated urine, Italian researchers have found.
"Radiologists should be familiar with the usual postoperative imaging appearances and the varied spectrum of possible complications, particularly to identify those occurrences that require prolonged in-hospital treatment or surgical reoperation," noted Dr. Massimo Tonolini and colleagues from the department of radiology at "Luigi Sacco" University Hospital in Milan, in an article published online on 10 September in Insights into Imaging. "Knowledge of the surgical procedure details, appropriate MDCT acquisition techniques, and special interpretation care are needed."
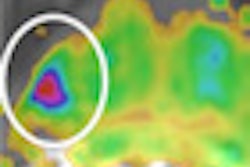
 Image from a triple-bolus MDCT urography acquisition in a 45-year-old postoperative patient shows simultaneous imaging of arterial, parenchymal, and excretory phases. This technique combined with preliminary unenhanced scans can allow time- and dose-efficient, reliable investigation of suspected iatrogenic injuries, including assessment of extraluminal blood, abnormal collections, active bleeding, urinary extravasation, and venous patency. All images courtesy of Dr. Massimo Tonolini.
Image from a triple-bolus MDCT urography acquisition in a 45-year-old postoperative patient shows simultaneous imaging of arterial, parenchymal, and excretory phases. This technique combined with preliminary unenhanced scans can allow time- and dose-efficient, reliable investigation of suspected iatrogenic injuries, including assessment of extraluminal blood, abnormal collections, active bleeding, urinary extravasation, and venous patency. All images courtesy of Dr. Massimo Tonolini.Robot-assisted laparoscopic radical prostatectomy (RALRP) is now the preferred minimally invasive surgical treatment for localized prostate cancer, with optimal oncologic and functional results, but severe complications can occur in 5% to 7 % of patients and sometimes require more surgery. In hospitals with an active urologic surgical service, imaging is increasingly valuable for assessing suspected early complications following RALRP surgery, they explained.
The authors have implemented advanced MDCT acquisition protocols to investigate the urinary tract, such as CT urography and split bolus techniques and CT cystography, and the small and large bowel, including CT enteroclysis, enterography, virtual colonoscopy, and water enema CT. The CT examination should be tailored to the patient and his/her clinical situation, and must aim to answer the referring physician or surgeon's questions and to limit the radiation dose as must as possible, according to Tonolini and colleagues, who believe it is important to acknowledge the inventors of the triple-bolus technique (Kekelidze M, et al. Kidney and urinary tract imaging: triple-bolus multidetector CT urography as a one-stop shop-protocol design, opacification, and image quality analysis. Radiology, May 2010, Vol. 255:2, pp. 508-516).
In their hospital, radiology nurses play a crucial role in developing, refining, and practicing these CT acquisition techniques, and their daily work is valuable in assuring a high-quality examination that is comfortable for patients.
For the last five years, the group has focused on different topics in abdominal imaging, especially chronic inflammatory bowel diseases, anorectal disorders, HIV-related conditions, and abdominal emergencies. In the field of urogenital imaging, they have concentrated on the role of advanced MDCT acquisition techniques such as split-bolus CT urography and CT cystography to investigate postoperative injuries following different open, laparoscopic, and percutaneous procedures.
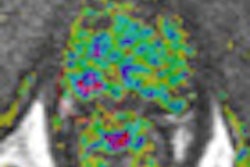
 Image from MDCT cystography acquisition in a 73-year-old postoperative patient after robot-assisted laparoscopic radical prostatectomy shows sufficient bladder distension and opacification of a minimal extraperitoneal leak at the vesico-urethral anastomosis (arrow). Applied with care in the early postoperative setting, this technique can allow confident detection or exclusion of urine extravasation indicating lower urinary tract injury both spontaneous (such as in colovesical fistulas from diverticulitis) and iatrogenic.
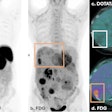
Image from MDCT cystography acquisition in a 73-year-old postoperative patient after robot-assisted laparoscopic radical prostatectomy shows sufficient bladder distension and opacification of a minimal extraperitoneal leak at the vesico-urethral anastomosis (arrow). Applied with care in the early postoperative setting, this technique can allow confident detection or exclusion of urine extravasation indicating lower urinary tract injury both spontaneous (such as in colovesical fistulas from diverticulitis) and iatrogenic.In urologic patients, a postoperative MDCT study should include a preliminary unenhanced acquisition to detect hyperattenuating blood and abnormal air collections, arterial and venous-phase images after intravenous contrast medium (CM) injection to assess the solid organs and identify extravascular CM indicating active bleeding, and excretory phase imaging. Images are obtained at least 5 minutes to 20 minutes (up to 1-2 hours) after CM, in order to demonstrate the opacified urinary cavities and detect iodinated urine leaks and urinomas, they wrote.
MDCT studies should be complemented with multiplanar reformations and 3D volume-rendered images to effectively depict the postoperative anatomy and salient findings. To limit the radiation dose during multiphasic acquisitions, the researchers have developed split-bolus MDCT urography protocols that allow for combined renal vascular, parenchymal, and excretory acquisition.
MDCT urography protocol should include preliminary unenhanced scans, an initial 30 mL CM bolus injected at 2 mL/s flow for urinary opacification, a seven minute delay, a second (50 ml at 1.5 mL/s), and third (65 mL at 3 mL/s) CM injection separated by 20 seconds to provide parenchymal and vascular visualization respectively, followed by a single MDCT volumetric acquisition.
When performed properly, triple-bolus MDCT urography can provide simultaneous renovascular, corticomedullary, nephrographic, and excretory imaging with a reduced effective radiation dose compared to the usual multiphasic MDCT protocols, they stated.
"Due to its intrinsically high contrast resolution, MRI provides excellent visualization of the normal postprostatectomy anatomy and of possible neoplastic recurrence. In the emergency setting, the use of MRI is limited by lengthy examination time, scanner availability, constraints, and artifacts in acutely ill patients," wrote the authors. "Compared to MRI, with appropriate acquisition techniques MDCT provides quicker reliable identification of blood collections, extravasated urine, and active bleeding. Furthermore, in patients with suspicion of VUA leak an additional focused investigation with conventional radiographic cystography or MDCT cystography is recommended."
In their department, diluted iodinated CM used during MDCT cystography is prepared by removing 40 mL to 50 mL of normal saline from a 500-mL bag and injecting a similar amount of nonionic contrast agent (e.g., 350 mgI/mL iomeprol or 370 mgI/mL iopromide) into the same saline solution bag. The bag is then connected to standard tubing for intravenous infusions, filling the tube with diluted contrast to avoid instilling air in the bladder. With the patient supine on the CT scanner table, slow retrograde infusion is obtained by gravity.
The injected CM volume should not exceed 150 mL, according to the group. The volumetric MDCT acquisition at sufficient bladder distension is visualized with multiplanar image reformations at CT angiography window settings (width 600-900 level 150-300 Hounsfield Units) and by maximum intensity projection or 3D techniques. The only potential pitfall of this technique is the possible occlusion of a limited anastomotic dehiscence by the Foley catheter balloon, they added.
Tonolini is currently putting the finishing touches to the proofs for a book about state-of-the art cross-sectional imaging of ulcerative colitis, which is due to be unveiled by Springer at the RSNA congress in November.