When neurosurgery is performed to resect a glioma, the use of intraoperative MRI guidance improves the chances the entire cancerous tumor will be removed. Patient outcomes from a randomized clinical trial confirmed this in an article published online on 24 August in Lancet Oncology.
A randomized clinical trial conducted at Goethe University in Frankfurt, Germany, confirmed the value of utilizing the technology with this neurosurgical procedure. Six months following surgery, the brain tumor had progressed in almost twice the number of patients who had conventional microsurgical resection compared with the patients who had the additional benefit of intraoperative MRI guidance during their surgery. And only half the number of patients who had conventional surgery were stable compared with patients in the intraoperative MRI guidance group.
The use of intraoperative MRI guidance enables surgeons to visualize tumor remnants that would not otherwise be seen and would remain unresected. It enables neurosurgeons to reassess neuronavigation during and throughout surgery. While surgeons performing conventional microsurgery use a neuronavigation system based upon preoperative imaging, anatomy is altered during surgery due to resection of tissue and loss of cerebrospinal fluid. These alterations can compromise the accuracy of conventional neuronavigation after dura opening and during tumor resection, with the potential for tumor remnants to be overlooked.
 A sample image showing the surgical setup, with the patient's head positioned in between the bores of the magnet; during surgery, imaging is repeated with sterile drapes placed around the head and the bores. All images courtesy of Dr. Christian Senft.
A sample image showing the surgical setup, with the patient's head positioned in between the bores of the magnet; during surgery, imaging is repeated with sterile drapes placed around the head and the bores. All images courtesy of Dr. Christian Senft.A total of 58 patients with known or suspected gliomas were enrolled to participate in the clinical trial between 1 October 2007 and 1 July 2010. Eight of these patients who were subsequently diagnosed as having metastases became ineligible for the study, and one patient withdrew from the trial, leaving a total of 24 patients randomly allocated to the intraoperative MRI group and 25 to the control group.
The majority of patients -- with 22 patients in each group -- had grade IV glioglastomas. The median preoperative tumor volumes were comparable, 17.7 cm for the intraoperative MRI group and 21.1 cm for the control group.
The use of MRI -- provided by a mobile intraoperative ultralow-field system (PoleStar, Odin Medical Technologies) -- during surgery led to extended tumor resection in one-third of the patients, according to lead author Dr. Christian Senft of the Klinik für Neurochirurgie and colleagues. All but one patient (96%) had a complete tumor resection compared with only 17 patients (68%) who had conventional microsurgery.
The conventional microsurgical procedure took a median of six hours, whereas the addition of intraoperative MRI extended the operation's duration by one hour. The surgeries were performed by both senior and junior neurosurgeons, but the level of experience had no impact on patient outcomes.
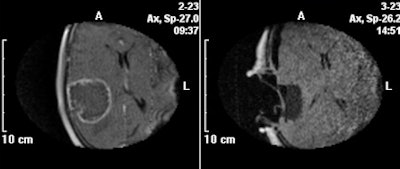 Exemplary T1-weighted contrast-enhanced images obtained at 0.15 tesla before (left) and after tumor resection (right), showing no residual tumor.
Exemplary T1-weighted contrast-enhanced images obtained at 0.15 tesla before (left) and after tumor resection (right), showing no residual tumor.All patients had an MRI examination both within a week and three days after surgery. Their images were reviewed by an experienced neuroradiologist to establish the extent of resection and to undertake volumetric analyses of the tumors and tumor residues. This radiologist was blinded to the patient group status.
Sixteen (67%) of the patients in the intraoperative MRI group were stable six months following surgery, compared with nine (36%) in the control group, the researchers reported. The disease progressed in eight (33%) patients in the MRI group, compared with 16 (64%) in the control group, one of whom had died.
While the clinical trial was designed to show the effect of intraoperative MRI guidance in ideal conditions and did not include an assessment of subsequent quality of life, the authors believe that the technique is comparable to the use of 5-aminolaevulinic acid, and is an appropriate method to improve the extent of resection of malignant brain tumors.