We invited three world experts to comment on the major milestones in radiation therapy research. When asked to choose a development of compelling benefit, one answer was unequivocal: image guidance.
Image guidance
When asked to choose a development that has been of compelling benefit to radiotherapy, one answer was unequivocal: image guidance. "I do think that volumetric image guidance has really been the major advance of the last five years," said Marcel van Herk, PhD, professor of medical physics at the University of Amsterdam and research medical physicist at the Netherlands Cancer Institute. "I think that imaging is making a major difference, because people are seeing what is going on inside the patients from day to day. I think that this is a major breakthrough."
 Marcel van Herk, PhD, University of Amsterdam
Marcel van Herk, PhD, University of Amsterdam
Professor Gino Fallone, PhD, director of the medical physics division of the department of oncology at Cross Cancer Institute in Edmonton, Alberta, Canada, concurred, highlighting the benefits provided by recent advances in magnetic resonance guidance. "I think that the advent of soft-tissue, real-time visualization for image guidance in radiotherapy, and also in proton therapy, is going to make a big, big difference to all of radiation oncology."
In the opinion of Professor Dirk Verellen, chief medical physicist of the Oncologic Center at Universitair Ziekenhuis Brussel in Brussels, it's hard to choose just one technology development that has made a difference. Rather, small steps have combined to provide a big step forward. "Image-guided radiotherapy, gated radiotherapy, adaptive radiotherapy -- these are all new developments, but they happened gradually because of the synergy of imaging with new computing power and new approaches in dose delivery," he said.
Verellen emphasized that as more precise dose distributions are delivered, more accuracy is needed in knowing exactly where that dose is delivered. "It's the combination of dose sculpting techniques and more accurate imaging during treatment that enables radiotherapy to become much more powerful," he explained. "Imaging can now be used to monitor a patient's response, allowing individual tailoring of future treatment factions."
Challenges today
 Professor Dirk Verellen, Universitair Ziekenhuis Brussel
Professor Dirk Verellen, Universitair Ziekenhuis Brussel
While image guidance has enabled many advances to take place, research efforts are ongoing. "If I give a talk at this moment about what we need in radiotherapy, it's imaging imaging and imaging. The top 10 priorities are imaging, all 10 of them. We need to see the tumor during treatment," Verellen said.
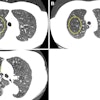
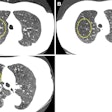
Real-time imaging can also help address another prominent issue in radiotherapy: target motion. This includes fast movement, such as respiration-induced shifts in the tumor and surrounding organs, where on-board imaging enables gating and tracking of moving targets. Imaging also helps visualize slower changes, such as tumor shrinkage and other anatomical deformations over the course of therapy. These effects can have the largest impact upon treatment outcome, according to van Herk.
A challenge that Verellen identified is that incremental technology advances can be hard to qualify. "The fact that it's little steps that together make a big difference means that there are no randomized trials. We are not trying to prove that a new approach is better than an old standardized approach, because there is no standardized approach. It's a gradual evolution. And that is maybe one of the frustrations of radiotherapy," he said.
What's next?
So how will radiotherapy technologies likely progress over the next few years? From van Herk's perspective, the next big challenge is not just for the medical physicists, it's for everybody working in the field of radiation oncology. "We are getting so good at hitting what we want to hit, that now the next major step is finding out what we actually want to hit," he said.
"I think that medical physicists should also be involved in radiology and magnetic resonance sequences and PET scanning. We have to have better images to know where the target is, and not try to be ultimately accurate at hitting something where we don't even know where it is," he added.
 Professor Gino Fallone, PhD, Cross Cancer Institute
Professor Gino Fallone, PhD, Cross Cancer Institute
Fallone pointed out that soft-tissue-based image guidance could allow radiation therapy to expand into new areas, enabling treatment of many disease sites that were not previously treatable.
Finally, Verellen highlighted the emergency of individualized treatment, aided by advances in functional imaging. In the past, treatment was not only population-based, but tumors were considered as a mass of homogenous cells, which is now known not to be the case. Rather, tumors are highly heterogeneous, with regions that respond well to radiation and radioresistant regions containing less oxygen that needed a boosted dose.
"Functional imaging allows us to look not only at the patient anatomy, but also the functions of tumors, so we can adapt our treatment to those regions," Verellen said. "We are not there yet. There's a lot of work to be done to be able to actually quantify this heterogeneity of the tumor. This quantification needs to be very accurate, and we're still sorcerer's apprentices in that field. But we're getting there, and that is the future."
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.