Even without typical risk factors, pulmonary thrombosis may be more prevalent than expected among those with acute trauma injuries associated with conflict, according to a study published on 20 August in European Radiology.
The study showed that these thromboses often occur without clinical suspicion or typical findings, with a high rate of missed diagnoses, and may be considered a clinical entity distinct from traditional venous thromboembolism.
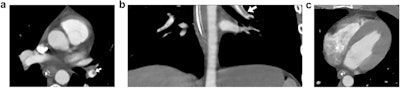 CT image of 31-year-old male soldier with gunshot wound who was treated with an IVC filter following identification of pulmonary arterial clots on the CT. The initial assessment included an abdominal trauma CT protocol covering only the lower chest. (a,b) Axial and coronal views show a filling defect within the left lower lobar artery consistent with a pulmonary thrombus (PT) (arrows). (c) Axial view of the heart: the right to left ventricular ratio is normal.Courtesy Aviram et al; European Journal of Radiology. Image available for republishing under Creative Commons license (CC BY-NC-ND 4.0).
CT image of 31-year-old male soldier with gunshot wound who was treated with an IVC filter following identification of pulmonary arterial clots on the CT. The initial assessment included an abdominal trauma CT protocol covering only the lower chest. (a,b) Axial and coronal views show a filling defect within the left lower lobar artery consistent with a pulmonary thrombus (PT) (arrows). (c) Axial view of the heart: the right to left ventricular ratio is normal.Courtesy Aviram et al; European Journal of Radiology. Image available for republishing under Creative Commons license (CC BY-NC-ND 4.0).
In a retrospective study, a team led by Dr. Galit Aviram of the Department of Radiology at Tel Aviv Sourasky Medical Center, Israel, analyzed immediate post-trauma CT scans of war-injured patients between the ages of 18 and 45. The scans were performed at two tertiary hospitals between 7 October 2023 and 7 January 2024, with the aim of investigating the prevalence and radiological characteristics of pulmonary thrombosis (PT) found with acute traumatic war injuries.
Additionally, the researchers aimed to assess the efficacy of a diagnostic AI algorithm used in these settings.
Recent studies have shown that venous thromboembolism, including PT, can develop shortly after traumatic injury. Moreover, this association with acute post-traumatic inflammation is “a fourth component to the genesis of thrombi beyond Virchow’s triad [i.e., the traditional thrombosis risk factors of hypercoagulability, abnormal blood flow, and endothelial damage],” the authors write.
The researchers retrospectively analyzed all consecutive CT scans performed at Tel Aviv Sourasky Medical Center and Sheba Medical Center for the initial assessment of traumatic injuries incurred by a cohort of 190 patients (183 men and 7 women, median age of 24, with a range of 21 to 30). None of the patients had possible risk factors for venous thromboembolism.
PT was detected in 10 patients, all of whom were men; the rate of PT in the cohort was therefore 5.6%. The median age of the PT group was 21.5 years (range, 20.75 to 28.75); the difference in ages between groups was not significant.
Of the CT scans, 111 (58.5%) consisted of full-chest imaging; the remaining scans were limited to lung apices or bases with contrast. For the group with PT, seven underwent the complete CT trauma protocol; the other three received partial lung field scans.
While a higher injury severity scale (ISS) was found in the patients with PT (21 [20-21] vs. 9 [4–14.5], respectively; p = 0.01), there were no significant differences between the groups for any other clinical, demographic, or laboratory data parameters.
There was a higher rate of lower extremity injuries in the PT group; however, the difference was not noted as statistically significant (70% in the PT group vs. 39.4% in the non-PT group; p = 0.094). Additionally, while there were no differences between the groups in the types of trauma, the injuries in the PT group were more complex.
There was no mortality after seven days among any of the 190 patients in both groups, the authors said.
Review with the AI algorithm revealed filling defects indicative of PT in five patients at each of the two centers, for a total of 10. At one center, four of the defects were flagged and reported at the initial reading by a senior radiologist; at the other center, none of the five cases were identified -- in other words, only 40% of the filling defects that were detected by the algorithm were initially reported and treated. There were no findings suggestive of right-ventricle dysfunction in any of the 10 cases, the authors add.
All identified patients underwent follow-up scans using a PE protocol after several months, none of which resulted in thrombus being detected.
The authors write that while hypocoagulability is considered typical in the early phase of trauma-induced coagulopathy, the findings suggest that the presence of hypercoagulability during the first 24 hours after injury should be examined more closely. Further, they suggest that the type of traumas inflicted -- i.e., those typical of war-related injuries -- should be examined in investigating this difference.
The authors conclude that PT in these cases appears as a distinct clinical entity; even with a high rate of PT (5.6%), none of the patients manifested radiological evidence of right ventricular dysfunction indicative of pulmonary embolism. Of particular concern, they add, is that 60% of these cases were not detected in real-time, suggesting that more education on this will be necessary, along with the development of specific protocols for this form of PT.
Read the study here.