CT perfusion (CTP) performed in combined PET/CT scans can provide valuable extra information about tumor behavior, and may help to differentiate between head and neck tumors and inflammatory lesions, Swiss researchers have found.
"PET/CTP can be integrated into a routine, contrast-enhanced PET/CT protocol for staging in ENT [ear, nose, and throat] cancers without additional use of contrast media," noted lead author Dr. Patrick Veit-Haibach, from the department of medical imaging at University Hospital Zurich, in an article published online by European Radiology on 9 July. "CTP and PET parameters were not significantly correlated, and hence the additional CTP values can provide additional insights into tumor behavior and their glycolytic status. Metastatic lymph nodes have high CTP values and can be possibly differentiated from the primary tumor lesion."
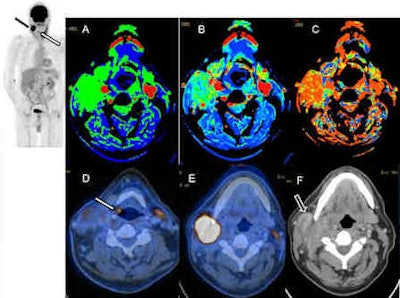 These images are of a 56-year-old man with suspected hypopharyngeal cancer and ipsilateral lymph node metastases. The maximum intensity projection (MIP) image (top left, white arrow) shows the small tumor at the aryepiglottic fold in the right side (D) with focal FDG avidity. Additionally, a large lymph node metastasis with high FDG activity was detected right cervically (black arrow on MIP image and E, F). Perfusion imaging of the large lymph node (A-C) shows elevated blood flow (A), blood volume (B), and also a decreased mean transit time (C). Images courtesy of Dr. Patrick Veit-Haibach.
These images are of a 56-year-old man with suspected hypopharyngeal cancer and ipsilateral lymph node metastases. The maximum intensity projection (MIP) image (top left, white arrow) shows the small tumor at the aryepiglottic fold in the right side (D) with focal FDG avidity. Additionally, a large lymph node metastasis with high FDG activity was detected right cervically (black arrow on MIP image and E, F). Perfusion imaging of the large lymph node (A-C) shows elevated blood flow (A), blood volume (B), and also a decreased mean transit time (C). Images courtesy of Dr. Patrick Veit-Haibach.The primary tumor and inflammatory lesions can be differentiated by CTP values, as well as partially by PET measurement, but further research (especially larger standardized studies) must focus on combined ratios of CTP and PET values to lead to a better understanding of the relation between tumor perfusion and glycolytic rate, according to the authors.
The prospective study included 41 patients with a clinically suspected head and neck cancer. All patients underwent a combined PET/CT with an integrated CTP examination in the area of the head and neck tumor. CTP and PET data were compared between the tumors and healthy contralateral tissue, inflammatory lesions, and metastatic lymph nodes, and CTP data and PET data were correlated in tumors.
All data were acquired on a combined PET/CT system (Discovery VCT, GE Healthcare). The patients were told to fast for four hours before the examination. PET/CT imaging with integrated CTP was started 60 minutes after the injection of a standard dose of 300-340 MBq of FDG. Blood sugar levels were checked prior to the injection of the FDG. In addition, an oral CT contrast agent -- 30 mL Gastrografin (Bayer Healthcare Pharmaceuticals) diluted with 970 mL water -- was administered during the uptake period.
Thirty-five patients had a head and neck cancer, the researchers discovered. All CTP data were statistically different between tumors, inflammatory lesions, healthy tissue, and metastatic lymph nodes; PET/CT data were in part significantly different. CTP and PET parameters were not significantly correlated.
"Since more hybrid PET/CT systems with perfusion capabilities are currently being installed, combined PET/CTP might find its way into clinical routine to support the diagnosis of malignant versus nonmalignant lesions," Veit-Haibach stated. "To achieve such a routine clinical level, it is first mandatory to find a cut-off value for the differentiation of malignant versus nonmalignant lesions based on perfusion parameters. However, to find such a generally accepted cut-off is complicated, because there are currently no guidelines and generally accepted technical specifications on how to perform perfusion imaging. Thus, such a cut-off value currently can only be used in a single center where it is evaluated."
In the Zurich study, which was partly supported by Bayer Healthcare, the mean blood flow for malignant lesions was 89.6 mL/100 mg/min and 68.6 mL/100 mg/min for inflammatory lesions. Since the blood flow for malignant lesions was comparable with other studies available in the literature, those values around 90 mL/100 mg/min (when evaluated with the same postprocessing software) might support the diagnosis of malignant rather than nonmalignant ENT lesions in questionable cases when the SUVmax does not clearly indicate malignancy, the authors wrote. However, they did not apply any further receiver operator characteristics (ROC) analysis because they thought the patient number for that is somehow limited, especially concerning inflammatory lesions.
The team is now working on several other areas, especially CT perfusion and PET/CT with integrated perfusion, Veit-Haibach explained. A study involving more than 100 patients with prostate cancer is under way, and is focusing on correlation with prostate-specific antigen (PSA), Gleason score, technical evaluations, and 50 patients for whom postsurgery comparisons are available. Other ongoing studies include 50 patients with PET/CT and integrated perfusion of bronchial carcinoma, and 30 patients with peripheral artery occlusive disease undergoing CT perfusion pre- and postangioplasty of the lower extremities.
|
Study disclosures The research was supported in part by a grant from Bayer Healthcare. |